Ascending aortic aneurysm is a localized dilation of the ascending aorta due to weakening of the vessel wall. It may remain asymptomatic for years but poses a high risk of rupture or dissection when enlarged. Screening is crucial in patients with risk factors such as hypertension or connective tissue disease.
Causes include genetic disorders like Marfan syndrome, bicuspid aortic valve, and chronic hypertension. Atherosclerosis and inflammatory conditions also contribute to aneurysm formation. Family history plays a significant role in predisposing individuals.
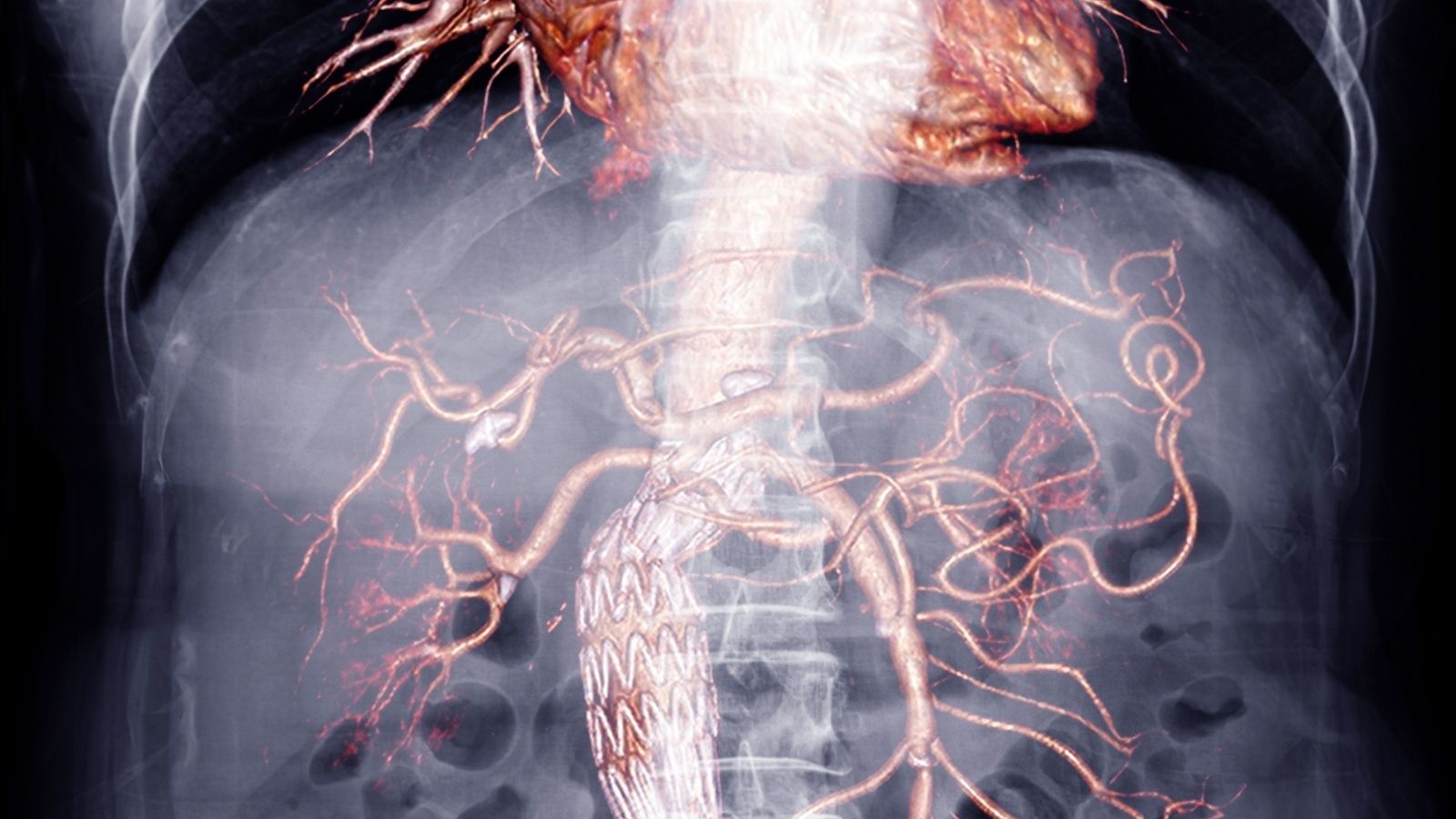
Diagnosis relies on echocardiography, CT angiography, or MRI to measure aortic dimensions. Regular imaging follow-up is essential to monitor aneurysm growth and determine the appropriate timing for surgical intervention.
Surgical repair is indicated when the aneurysm exceeds a critical diameter or shows rapid progression. Techniques include open replacement with a synthetic graft or endovascular repair in selected patients. Timely surgery prevents life-threatening rupture and dissection.
| Definition | Abnormal enlargement of the first part of the aorta (ascending aorta), which originates from the heart |
| Causing Factors | Hypertension, connective tissue diseases (Marfan syndrome, Ehlers-Danlos syndrome), bicuspid aortic valve, aortitis, genetic predisposition |
| Risk Factors | Age, male gender, smoking, family history, uncontrolled hypertension |
| Symptoms | Usually asymptomatic; chest pain, shortness of breath, difficulty swallowing may be observed in large aneurysms |
| Diagnostic Methods | Echocardiography (TTE/TEE), CT angiography, MRI, chest radiography |
| Complications | Dissection, rupture, aortic valve insufficiency, thrombosis, embolism |
| Treatment Methods | Medical follow-up and blood pressure control in small aneurysms; surgical repair (aortic graft) in large or symptomatic aneurysms |
| Tracking and Monitoring | Chaplain monitoring with regular imaging (CT/MRI), blood pressure control, cardiology follow-up |
| Ways to Intercept | Control of hypertension, smoking cessation, regular screening (especially in high-risk individuals) |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is an Ascending Aortic Aneurysm and where does it affect the body?

An ascending aortic aneurysm is a permanent enlargement or ballooning of the beginning part of the aorta, the main artery that leaves the heart, due to a structural weakness in the vessel wall.
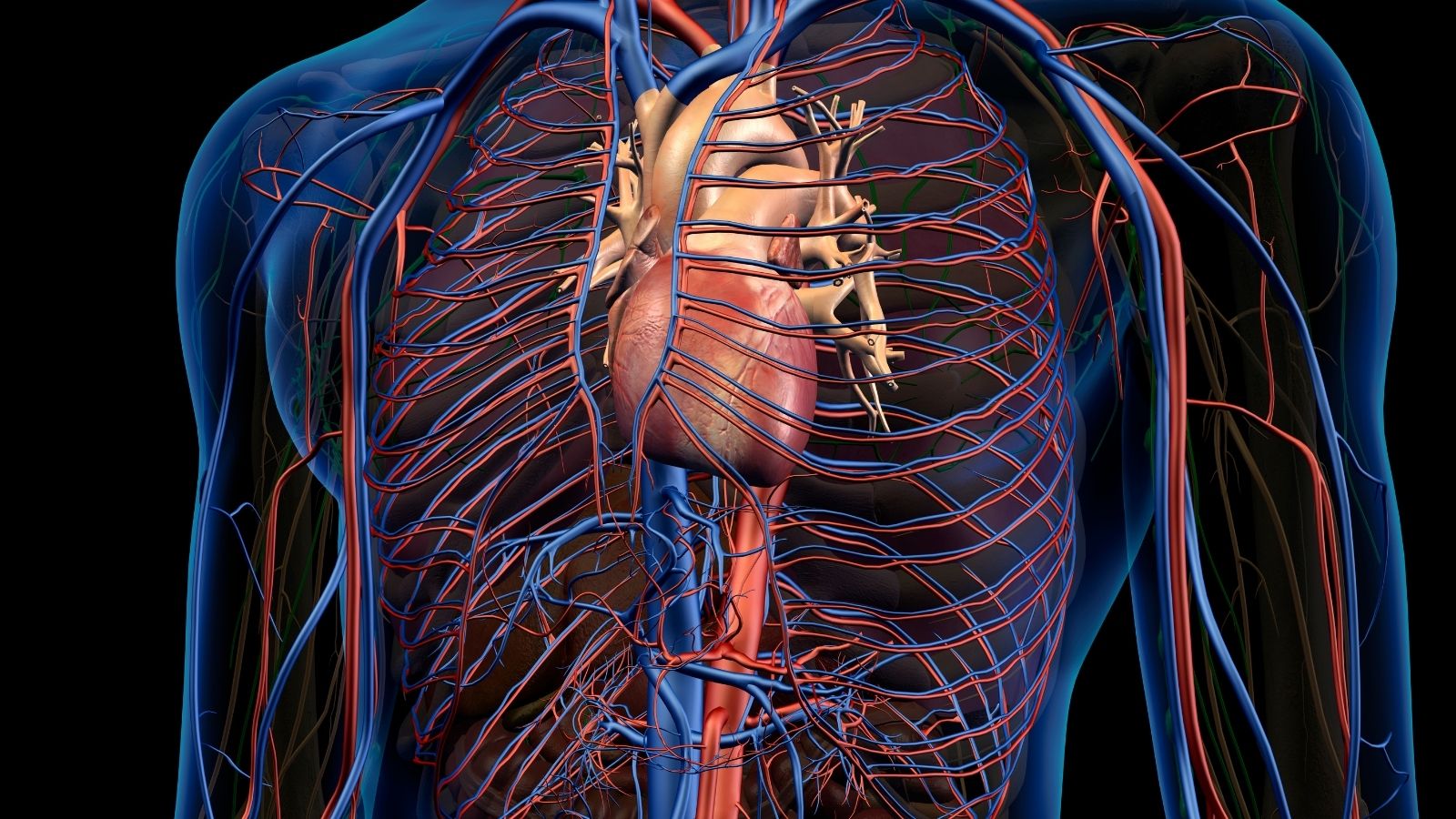
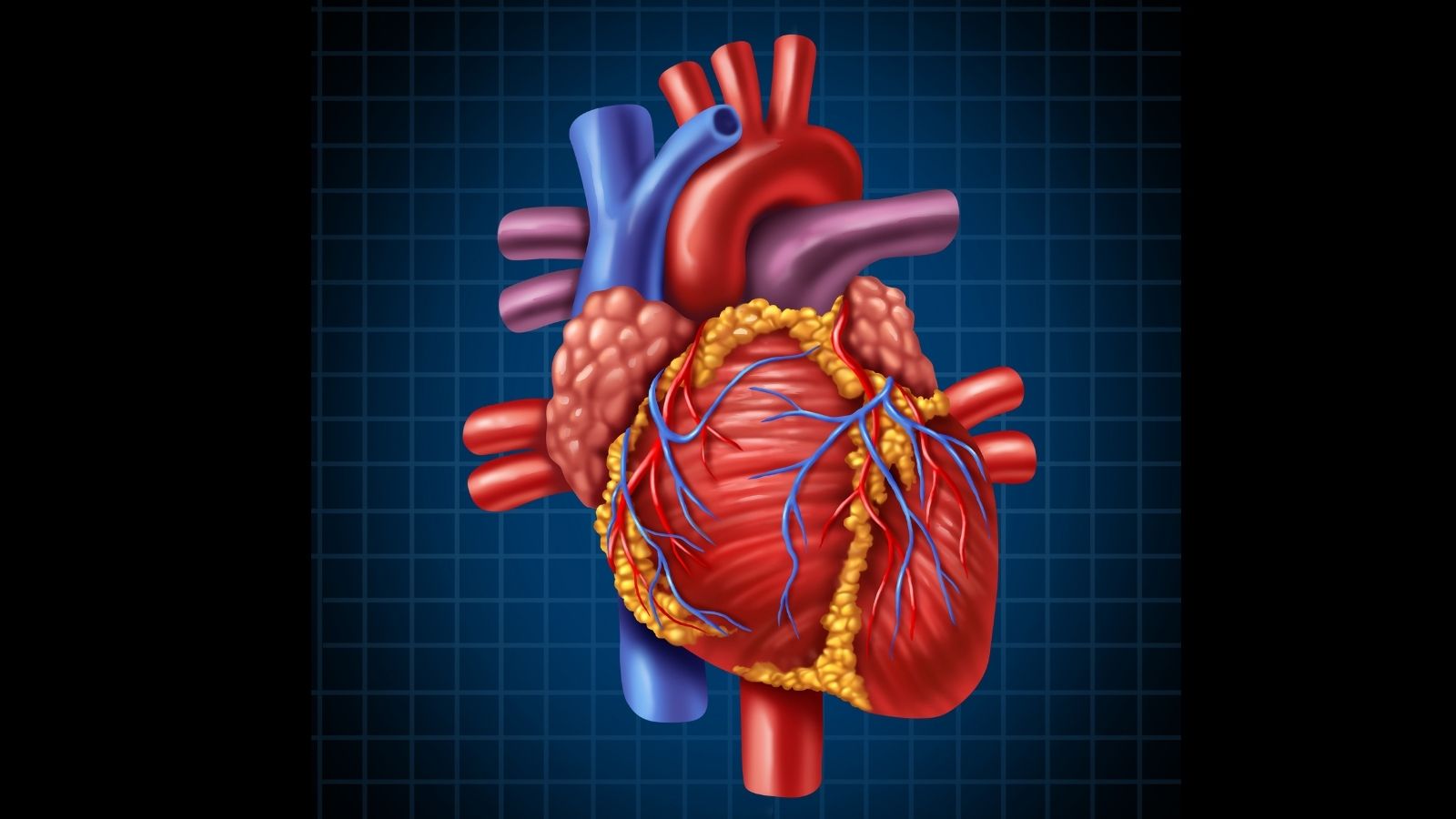
The aorta can be compared to a walking stick with a curved end. It exits the heart, makes a curve and travels downward through the chest and abdominal cavity. The ascending aorta is the first and most critical part of this structure, coming immediately after the heart and heading upwards. It is located just behind our breastbone and contains the aortic valve, which regulates the blood flow to our heart, and the aortic root, which also contains the exit points of the coronary vessels that supply the heart. An ascending aortic aneurysm is therefore a condition that affects precisely this vital area.
In medicine, we call an aneurysm an enlargement of the diameter of a blood vessel that is 1.5 times (P) larger than the normal diameter that it should be according to a person’s age and body size. For lesser dilatations, we use the terms “dilatation” or “ectasia”. To give a practical example, a diameter of 4 cm or more in the ascending aorta is usually considered a dilatation, while a diameter of 5 cm or more in a person under 60 years of age is now considered an aneurysm. Ascending aortic aneurysms account for approximately ` of all aortic aneurysms seen in the chest cavity and are the most commonly encountered type.
How does an Ascending Aortic Aneurysm develop in the vessel wall?
The underlying mechanism of an ascending aortic aneurysm is quite different from atherosclerosis, which we usually see in abdominal aneurysms. Almost all of these aneurysms are caused by a process known as “cystic medial degeneration”. We can think of it as a structural collapse of the middle layer of the aortic wall, almost like a jelly-like weakening.
The aortic wall consists of three layers. The middle layer (the media) is a network of neatly arranged elastin fibers that give the vessel its elasticity and resistance to pressure, and smooth muscle cells that constantly repair this structure. The development of an aneurysm involves a series of disruptions in this network:
- The elastin fibers that give the wall its elasticity become shiny and thin.
- The smooth muscle cells that keep the wall alive and intact, and that carry out constant repair, begin to die.
- The supporting tissue that forms the structural skeleton of the wall is actively broken down by some specialized enzymes.
- These intact structures are replaced by a gel-like substance that reduces the resistance of the wall.
This chain of cellular events weakens the vessel wall. A simple law of physics comes into play here: The larger the diameter of a pipe, the greater the stress on the wall caused by the pressure inside it. So as the aneurysm begins to expand, the stress on the wall increases. This increased stress leads to further deterioration of the wall and further expansion. This is a dangerous shortcut that explains why the aneurysm continues to grow steadily over time.
What are the risk factors for the development of ascending aortic aneurysm?
An ascending aortic aneurysm does not occur for a single reason. It is usually the result of a complex interaction of factors such as genetic predispositions, congenital heart defects and lifelong exposure to high blood pressure. These risk factors may differ depending on the age of the patient.
In young patients, congenital factors are usually predominant:
- Marfan syndrome
- Loeys-Dietz syndrome
- Ehlers-Danlos syndrome (vascular type)
- Bicuspid aortic valve (congenital two-leaf aortic valve)
- Familial aneurysm predisposition (FTAAD)
- Turner syndrome
In older patients, on the other hand, usually acquired, deterioration-related factors are more common:
- Advanced age (most common factor)
- Hypertension (high blood pressure)
- Smoking (the most important modifiable risk factor)
- Atherosclerosis (arteriosclerosis)
How do genetic syndromes increase the risk of Ascending Aortic Aneurysm?
Syndromes such as Marfan, Loeys-Dietz and vascular Ehlers-Danlos are caused by defects in genes that code for the connective tissue that forms the structural skeleton of our body. This causes the aortic wall to be inherently weak and flimsy, which makes a person extremely susceptible to developing an aneurysm.
In patients with these syndromes, aneurysms usually occur at a much younger age, grow more rapidly and, most importantly, are at risk of rupture even in smaller diameters. That is why patients with one of these diagnoses need to be followed much more closely and the decision to operate should be made at an earlier stage, in smaller aneurysm diameters. For example, while surgery is normally recommended for an aneurysm with a diameter of 5.5 cm, in a patient with Marfan syndrome this limit can be reduced to 4.5-5.0 cm, and in a patient with Loeys-Dietz syndrome to 4.0 cm.
Can Ascending Aortic Aneurysm show a familial predisposition?
Yes, absolutely. Ascending aortic aneurysm and dissection can be genetically transmitted directly between family members, even in the absence of a distinct syndrome. We call this condition “Familial Thoracic Aortic Aneurysm and Dissection (FTAAD)”.
Studies have shown that approximately one in five patients with a thoracic aortic aneurysm has a family history. This makes it clear that the tendency to develop aneurysms has a genetic component. Therefore, when a patient is diagnosed with an ascending aortic aneurysm, it is critical for us to take a detailed family history. If there is a family history of an aneurysm in another member or a sudden and unexplained death at a young age, this requires that all first-degree relatives of the patient (parents, siblings and children) also undergo an aortic screening. This proactive approach can save the lives of other at-risk family members.
What is the relationship between a bicuspid aortic valve and ascending aortic aneurysm?
The bicuspid aortic valve, which has two leaflets instead of three at birth, is one of the most important risk factors for ascending aortic aneurysm. This is the most common congenital heart anomaly, affecting approximately 1-2% of the population. Up to a percentage of patients with a bicuspid valve may develop an enlarged aortic artery at some point in their lives.
There are two main theories underlying this powerful relationship. The first is abnormal blood flow. Whereas a normal valve directs blood in an orderly fashion towards the center of the aorta, a bicuspid valve drains blood in a turbulent and asymmetrical fashion, like a water jet, directly into the aortic wall. Over the years, this constant mechanical stress weakens that area of the wall and causes it to expand.
The second theory is a genetic predisposition. The bicuspid valve and the ascending aorta are formed from the same stem cells during development in the womb. Because of this common origin, it is thought that a genetic “defect” in the valve leads to an innate weakness in the aortic wall. As a result, a genetically weak aortic wall is subjected to constant mechanical stress from abnormal blood flow and expands over time. Therefore, it is vital that every patient with a diagnosis of a bicuspid valve is followed regularly for aneurysm development, even if valve function is normal.
What symptoms does an ascending aortic aneurysm cause?
Ascending aortic aneurysms usually cause no symptoms until a life-threatening complication such as rupture or dissection develops. This “silent” nature is the most dangerous aspect of this disease. An aneurysm is usually detected completely by chance during imaging tests performed for another reason (e.g. a chest X-ray taken for a suspected pneumonia or an ultrasound of the heart during a check-up).
However, when the aneurysm is very large, it can start to put pressure on neighboring organs in the chest. Symptoms that can be seen in this situation are as follows:
- A dull, deep, aching pain felt in the chest or back
- Shortness of breath or dry cough caused by pressure on the trachea
- Voice loss caused by pressure on the nerve that controls the vocal cords
- Swallowing difficulty as a result of pressure on the esophagus
If the aneurysm ruptures or dissects, the symptoms are sudden, very severe and dramatic. This is an absolute medical emergency and 112 should be called immediately. These life-threatening symptoms include:
- A sudden, excruciating pain in the chest or back, described as “stabbing” or “tearing”
- Dizziness, lightheadedness or fainting caused by a sudden drop in blood pressure
- Severe and sudden onset of shortness of breath
- Stroke symptoms such as weakness on one side of the body, speech impairment
What methods are used for the diagnosis of ascending aortic aneurysm?
The diagnosis of ascending aortic aneurysm is confirmed by imaging tests performed on suspicion. We use three basic imaging methods to measure the size of the aneurysm, determine its shape and formulate a treatment plan:
- Echocardiography (ECHO): This is an ultrasound method using sound waves. It is non-invasive, radiation-free and easy to perform. It is an excellent screening and follow-up tool, especially to assess aortic root and the beginning of the ascending and descending aorta, as well as the structure (e.g. whether it is bicuspid) and function of the aortic valve (whether or not it is cusped).
- Computed Tomography Angiography (CTA): It is the “gold standard” in aneurysm evaluation. It is fast and shows the entire aortic vessel from start to finish with high resolution, three-dimensional images. It provides the most detailed and reliable information for surgical planning. However, it requires the use of an iodinated contrast medium and radiation exposure. It is very important that the acquisition is synchronized with the heart rhythm (ECG-gated) to avoid measurement errors.
- Magnetic Resonance Angiography (MRA): Provides high resolution images without the use of radiation or iodinated contrast media. Thanks to this feature, it is a method we often prefer, especially in young patients or in cases that require close follow-up.
Accurate and consistent measurement is the foundation of aneurysm management. Therefore, using the same method in all subsequent examinations and performing measurements from standard anatomical points is of great importance for us to make the treatment decision correctly.
When does the risk of rupture or dissection of an Ascending Aortic Aneurysm increase?
There are some important factors that allow us to assess the risk of an aneurysm rupturing or dissecting. This risk assessment is the most important step in determining when we should refer a patient for surgery. The main risk-enhancing factors are:
- Maximum diameter (size) of the aneurysm
- Annual growth rate of an aneurysm
- Presence of an underlying genetic syndrome (such as Marfan, Loeys-Dietz)
- Family history of aortic dissection or rupture
- Uncontrolled high blood pressure
- Smoking
The most critical of these factors is aneurysm diameter. As the diameter increases, the risk of rupture and dissection increases exponentially as wall tension also increases. Especially when the diameter exceeds 5.5 cm, the risk increases significantly. 6.for aneurysms larger than 0 cm, the annual risk of rupture reaches 7%. Likewise, rapid aneurysm growth (more than 0.5 cm per year) is an indication that the wall is unstable and is an important alarm sign, regardless of the diameter.
What does a “watchful waiting” strategy for ascending aortic aneurysm involve?
“Watchful waiting” or active surveillance is the standard approach for small, slow-growing aneurysms (usually less than 5.0-5.5 cm) that have not reached a size that requires surgery. This is not “wait and see”; rather, it is an active process aimed at closely monitoring the behavior of the aneurysm and proactively managing the risks. There are key components to this strategy:
- Regular imaging follow-up at defined intervals (usually once a year with MRA, CTA or ECHO)
- Keeping blood pressure tightly controlled with medication (target usually below 130/80 mmHg)
- Managing lifestyle risk factors
- Lifestyle management is particularly important and includes
- Absolute cessation of smoking
- Avoid heavy lifting (more than 10-15 kg), work that requires pushing and competitive sports
- Encouraging moderate aerobic exercise such as walking and swimming
- Adopting a heart-healthy diet, low in salt and saturated fat
When does an ascending aortic aneurysm require surgery?
The decision to operate is one of the most critical decisions in aneurysm management. We make this decision when the aneurysm has reached a point where the risk of rupture or dissection is greater than the risk of the surgery itself. The goal is to intervene at the safest time, before disaster strikes. According to current international guidelines, the thresholds for general surgery are as follows:
- Aneurysm diameter reaching 5.5 cm in people without any risk factors
- Diameter reaching 5.0 cm in those with risk factors such as Marfan syndrome or family history
- Diameter reaching 4.0-4.5 cm in very aggressive cases such as Loeys-Dietz syndrome
- Diameter reaching 5.0 cm in patients with bicuspid aortic valve and additional risk factors
- Growth of the aneurysm by more than 0.5 cm per year, regardless of the aneurysm diameter
- The appearance of symptoms such as pain due to an aneurysm, regardless of the aneurysm
If a patient with a bicuspid valve already needs surgery for valve replacement, aneurysm repair is also performed in the same session, even if the aneurysm diameter is as small as 4.5 cm.
What kind of life awaits patients after ascending aortic aneurysm surgery?
| The Progression of Renewal | Average 15-20 days; may vary depending on the extent of surgery and accompanying conditions. |
| Physical Activity | Light walking is recommended for the first 6-8 weeks; heavy lifting and pushing are prohibited. |
| Blood Pressure Control | To reduce pressure on the aorta, the ideal blood pressure should be kept below 140/80 mmHg. |
| Drug Use | Beta-blockers, ACE/ARB group drugs and, if necessary, blood thinners are given. |
| Nutrition | A low-sodium, low-fat, vegetable-fruit, high-fiber diet is recommended. |
| Imaging Monitoring | Follow-up with CT angiography or MRI is required 3-6 months postoperatively and once a year thereafter. |
| When Valve Replacement is Associated | Additional medication and monitoring requirements arise; INR monitoring may be required. |
| Complications | There is a risk of pseudoaneurysm, problems with the prosthesis site, arrhythmia, re-development of aneurysm. |
| Infection Prevention | Hygiene and monitoring are important due to the risk of chest bone infection and wound infection. |
| Sexual Activity | Once blood pressure control is achieved, it is usually possible within 4-6 weeks. |
| Psychological Status | Anxiety and depression may occur; it is useful to seek psychological support. |
| Smoking and Alcohol | Strongly not recommended; it is harmful to aortic health. |
| Tool Usage | it should be started after 4-6 weeks; when concentration and physical improvement are complete. |
| Controls | Cardiology and cardiovascular surgical follow-up should be maintained regularly throughout life. |
Long-term outcomes after elective ascending aortic aneurysm surgery are extremely disappointing. Patients who successfully survive the first critical postoperative period have a life expectancy similar to healthy people their own age, and their quality of life is usually very good.
But treatment does not end with surgery. Surgery solves the existing problem but does not completely eliminate the underlying vascular disease tendency that led to the aneurysm. Therefore, it is necessary to take some steps that will last a lifetime to maintain a healthy life after surgery and prevent future risks.
The recovery process usually starts with a 5-10 day stay in hospital. Full recovery at home and union of the breast bone can take 2-3 months. There are some rules to follow during this period:
- not lifting, pushing or pulling anything heavier than 5-10 kg for 4-6 weeks
- Not driving for at least 3-4 weeks
- Keeping the wound clean and dry
- Regular use of medicines prescribed by the doctor
Lifestyle changes after surgery are not only part of the recovery process, but also a lifelong commitment to protect the entire vascular system. Among these changes are the following:
- Quit smoking completely
- Keeping blood pressure and cholesterol under control
- Following a heart-healthy diet
- Incorporate safe, moderate physical activity into your life as recommended by your doctor
Finally, lifelong follow-up after surgery is vital. Even if the operated area is intact, other parts of the aorta (aortic arch, descending aorta or abdominal aorta) may enlarge over time. To monitor this risk, a lifelong follow-up program is established, usually involving periodic imaging with CTA or MRA and regular clinical evaluations by a specialist.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.