Arteriovenous malformation (AVM) is a vascular anomaly where abnormal connections between arteries and veins bypass the capillary system. This leads to turbulent blood flow, increased pressure, and a risk of rupture or bleeding in affected tissues.
Clinical manifestations depend on AVM location. Cerebral AVMs may cause headaches, seizures, or hemorrhagic stroke, while peripheral AVMs present with swelling, pain, or skin changes. Diagnosis relies on advanced imaging techniques such as MRI and angiography.
Treatment strategies include microsurgical removal, endovascular embolization, or stereotactic radiosurgery. The choice depends on AVM size, location, and patient condition. Multidisciplinary management ensures the best therapeutic outcomes.
Long-term care involves regular imaging follow-ups to monitor recurrence or residual malformations. Patients are also advised to manage blood pressure and avoid risk factors that could trigger bleeding. Early detection and treatment significantly reduce complications.
| Medical Term | Arteriovenous Malformation (AVM) |
| Definition | Congenital vascular anomaly lacking a normal capillary bed with direct connections between arteries and veins |
| Places of Occurrence | Most commonly in the brain and spinal cord; can also be seen in the skin, lungs, liver and extremities |
| Main Causes | Congenital (congenital) developmental anomaly – Rarely acquired |
| Symptoms (Brain AVM) | Headache, epileptic seizures, focal neurological signs, loss of consciousness, stroke symptoms |
| Symptoms (Peripheral AVM) | Pulsating mass, skin redness, increased temperature, pain, ulceration, bleeding |
| Complications | Intracranial hemorrhage, congestive heart failure (in high-flow AVMs), neurological damage |
| Diagnostic Methods | Brain AVM: MRI, MRA, CT angiography, cerebral angiography – Peripheral AVM: Doppler USG, CT/MR angiography |
| Treatment Methods | Surgical resection, endovascular embolization, stereotactic radiosurgery (especially in brain AVMs) |
| Follow-up Process | Regular imaging and neurological evaluation is recommended in symptomatic and high-risk AVMs |
What is AVM Disease and how does it affect our body?
AVM disease is the presence of this abnormal vascular network, especially in sensitive organs such as the brain and spinal cord. Normally, blood passes from the arteries to the capillaries, slowing down and nourishing the tissues. In AVM, this capillary network is absent. High-pressure blood rushes from the artery directly into a thin-walled vein that cannot withstand this pressure. This abnormal junction is called a “nidus” or tangle.
The way this condition damages the body, especially the brain, relies on three basic mechanisms. The first is that the AVM “steals” blood from the surrounding healthy brain tissue. Because blood prefers to flow towards this abnormal tangle where there is little resistance, neighboring brain cells are deprived of the oxygen and nutrients they need. Because of this “stealing phenomenon”, even if the AVM did not bleed, over time the brain cells in that area can weaken and die. This can manifest itself in symptoms such as seizures or slowly progressive weakness.
The second effect is that the AVM tangle grows over time and acts like a mass. This growing lump can put pressure on important centers of the brain such as speech, movement or vision. This pressure can also disrupt the circulation of the cerebrospinal fluid that protects the brain, causing a dangerous increase in pressure inside the skull (hydrocephalus).
The third and most feared effect is bleeding. The walls of the veins cannot withstand this intense pressure from the arteries. Over time, they weaken, expand, balloon (develop an aneurysm) and eventually rupture. This is a cerebral hemorrhage and is called a hemorrhagic stroke. This sudden bleeding is often the first reason for patients to consult a doctor. Therefore, the answer to the question “are vascular tangles in the brain dangerous?” is unfortunately yes. The risk of bleeding involved makes AVM a very dangerous condition.
What are the different types of AVM disease and where is it most common?
Although AVMs can occur almost anywhere in the body, the most common and most important ones are those found in the central nervous system. There are various types depending on their location and structure. The main types of shopping centers are:
- Brain Malls
- Spinal cord malls
- Peripheral AVMs (in the arms, legs, face or internal organs)
- Dural Arteriovenous Fistulas (DAVF)
- Vein of Galen Malformation (VOGM)
Brain AVMs are the most common of these types. The location of the AVM in the brain directly determines the symptoms it causes. For example, an AVM in the back part of the brain, which is related to vision, can cause visual field loss, while an AVM in a region related to movement can lead to weakness in the arm or leg.
Spinal cord AVMs are rarer but can cause serious problems, including back pain, progressive weakness and numbness in the legs and even paralysis.
The most critical point to understand here is this: What matters more than the size of a shopping mall is how much “valuable” land it occupies in the brain. We call the areas that govern vital functions such as speech, comprehension and movement “eloquent” or functionally important areas. A small AVM in these areas can be much more dangerous than a larger AVM in a quieter part of the brain, and its treatment is just as risky. Therefore, each patient’s condition is as unique as a fingerprint and the treatment plan is individualized.
What causes AVM disease and what factors increase the risk of bleeding?
The vast majority of AVMs are thought to be congenital, i.e. a “manufacturing defect” in the vascular system that occurs during development in the womb. It is not known why some people develop this defect. It is usually not hereditary, meaning that it is not passed on directly from parent to child. However, the incidence of AVMs is increased in some rare genetic diseases such as Osler-Weber-Rendu syndrome (HHT).
Although the presence of an AVM is a risk in itself, not all AVMs have the same risk of bleeding. But is AVM disease fatal? The answer to this question depends on the risk factors of the AVM. There are some important factors that increase the likelihood of an AVM bleeding:
- Previous bleeding
- Located deep in the brain
- Draining blood into veins deep in the brain
- Presence of additional aneurysms (bubbles) within the tangle or on the feeding vessel
The presence of any of these factors increases the annual risk of bleeding above the general average of 2-4%. In particular, a previously bleeding AVM carries the highest risk. The likelihood of rebleeding within a year of the first bleeding is quite high. Therefore, a patient’s actual risk is calculated individually based on these characteristics. This explains why some patients are told to “wait and see” while others are offered urgent treatment.
What are the symptoms of AVM disease?
Many people with AVMs may have no symptoms their whole lives and the condition may be discovered by chance during a brain scan for another reason. However, when symptoms do occur, they differ depending on whether the AVM is bleeding or not.
An AVM that has not yet bled can give various symptoms depending on its location and size:
- Seizures (epilepsy)
- Throbbing or migraine-like headaches, usually unilateral
- Increasing muscle weakness or numbness on one side of the body
- Vision problems (blurred vision, double vision, visual field loss)
- Dizziness, difficulty with balance and coordination
- Difficulty speaking or understanding what is being said
- Memory, planning and concentration problems
- Rarely, a buzzing sound (bruit) that can only be heard with a stethoscope or felt by the patient
Hemorrhage caused by AVM rupture causes much more sudden and severe symptoms and requires urgent medical intervention:
- sudden onset and excruciating headache, described as “the worst headache of my life”
- Nausea and vomiting
- Neck stiffness
- Hypersensitivity to light
- Unconsciousness, drowsiness or complete loss of consciousness (coma)
The most important message to remember here is this: Mild or absent symptoms do not mean that the AVM is not dangerous. Some AVMs with the highest risk of bleeding can remain completely silent until they rupture. The measure of safety is not how the patient feels but the anatomical features of the AVM as revealed by imaging methods.
How is AVM disease diagnosed?
When AVM is suspected in a patient, the diagnostic journey usually involves several steps. This process is similar to putting the pieces of a puzzle together to get a complete picture. The first step is to listen carefully to the patient’s complaints and perform a detailed neurological examination. Modern imaging technologies are used for definitive diagnosis.
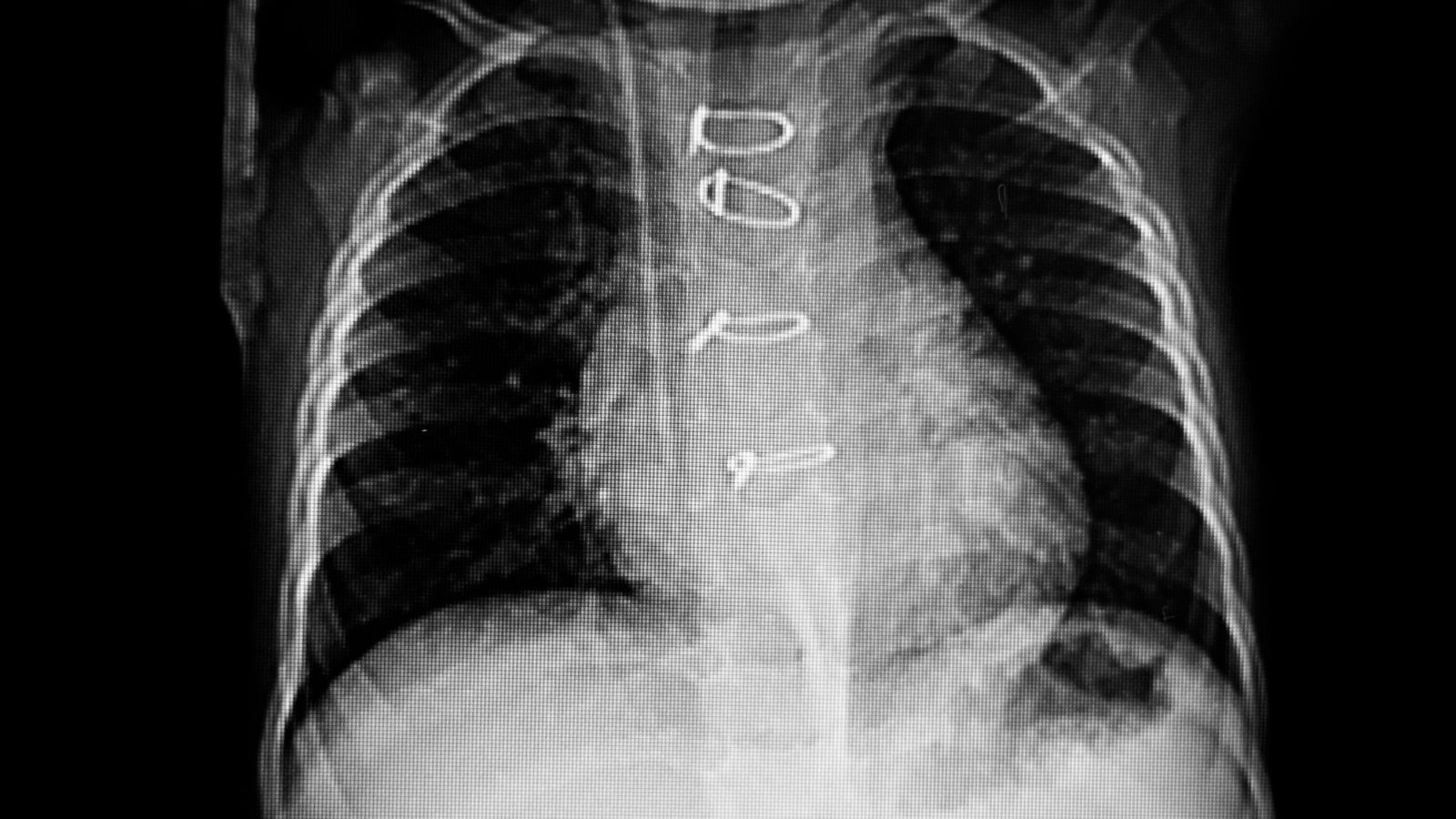
Computed Tomography (CT) is usually the first test used. In a patient who comes to the emergency room with a sudden and severe headache, CT can show within seconds whether there is a brain hemorrhage. If there is no bleeding or if a more detailed examination is needed, the next step is Magnetic Resonance Imaging (MRI). MRI shows the soft tissue of the brain and the AVM tangle itself in much more detail. It allows us to understand where the mall is located, its size and its neighborhood with important centers of the brain.
However, the gold standard method for planning AVM treatment is Cerebral Angiography (DSA). This is a type of vascular x-ray. A very thin catheter is inserted through an artery in the groin or wrist to reach the brain vessels. A special dye is injected through the catheter and a film of the blood vessels is taken. The angiography provides us with a road map of the AVM: it clearly shows which arteries supply it, how complex the internal structure of the tangle is and which veins drain the blood. Without this detailed map, it is not possible to plan a safe and effective treatment.
How is brain AVM disease graded and why is this important?
Not all AVMs have the same risk and difficulty of treatment. Therefore, surgeons use a standardized system to objectively assess the risk of surgery in particular. The best known of these systems is the Spetzler-Martin Grading System. This system expresses the complexity and surgical risk of AVM with a score from 1 to 5. Scoring is based on three main criteria:
- Size of the AVM nodule (nidus)
- Functional importance of adjacent brain tissue (whether it is in a valuable area)
- Deep or superficial veins draining the blood
The grade of the AVM is determined by adding the scores obtained from these three criteria. Low-grade (Grade I-II) AVMs have the lowest risk of surgery. High-grade (Grade IV-V) AVMs are the most challenging and risky cases; in these cases, non-operative methods or combined treatments are usually preferred.
This rating system is a universal tool that allows doctors to speak the same language across the world. It allows them to explain why a patient is recommended a particular treatment with concrete data. instead of a general statement such as “Your surgery is risky”, saying “Your AVM is Grade IV because it is large and close to the movement center of the brain, so we will first try another method to reduce the risk” allows the patient to participate more consciously in the treatment process.
What are the treatment options for AVM Disease?
There is no one-size-fits-all prescription for AVM treatment. The decision is like balancing the risk of bleeding in the natural course of the disease against the risks of treatment. Many factors such as the patient’s age, general health and the extent and location of the AVM are considered together to find the best option. The main treatment approaches are:
- Observation and Monitoring
- Surgical Resection (Surgical Removal)
- Endovascular Embolization (Intravascular Occlusion)
- Stereotactic Radiosurgery (Focused Beam Therapy)
In modern AVM treatment, these methods are often used together as part of a strategy rather than in isolation. For example, before operating on a large AVM, embolization can be used to block some of the vessels feeding the tangle, making it smaller and safer to operate on. Or radiosurgery may be used for a residual fragment that cannot be removed by surgery. Treatment can therefore be a journey of several steps rather than a single procedure.
When is surgical resection considered in the treatment of AVM disease?
Surgical resection, i.e. the complete removal of the AVM tangle by open brain surgery, is the most precise and immediate method to get rid of this disease. When successfully completed, it immediately and permanently eliminates the risk of bleeding. For this reason, it is considered the gold standard treatment, especially for low-grade AVMs that are close to the surface of the brain and can be safely reached surgically. For AVM patients, a successful operation means that the disease is completely cured.
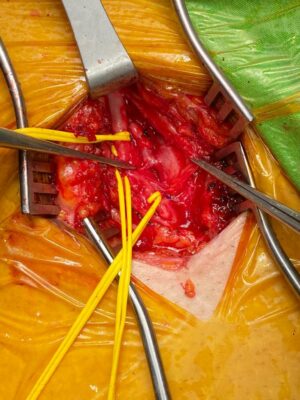
The surgery is performed under general anesthesia using an operating microscope. The surgeon separates the AVM tangle from healthy brain tissue with the precision of a sculptor. He first finds and closes the arteries that feed the tangle, then removes the tangle and finally cuts the veins that drain the blood. The basic principle of surgery is “all or nothing”. The goal is to remove the entire tangle, because even a tiny piece left behind can mean that the risk of bleeding continues or even increases. This reassures the patient that if the surgeon feels unable to completely remove an AVM, he or she will recommend another safer treatment alternative.
What is the role of endovascular embolization in the treatment of AVM disease?
Endovascular embolization is a less invasive method that does not require open surgery. It is similar to a plumber repairing a blocked or problematic pipe from the inside with special materials without breaking the wall. In this procedure, an interventional neuroradiologist inserts a very thin and flexible catheter through an artery in the groin or wrist and into the vessels of the brain, directly into the AVM.
Once the catheter is in the right place, a special liquid glue called Onyx or tiny metal coils (coils) are injected through it. This material blocks the vessels supplying the AVM, reducing or completely stopping the blood flow through it. Embolization alone rarely provides a complete cure. Its main role is to help with other treatments. It is used for strategic purposes, such as reducing blood flow in an AVM before surgery to make surgery easier, or shrinking a large AVM before radiosurgery to make radiation therapy more effective. Its success is measured not by how well it eliminates the AVM, but by how safe and effective it makes the next actual treatment.
Which AVM disease cases are suitable for stereotactic radiosurgery?
Stereotactic radiosurgery (Gamma Knife or similar technologies), despite the word “surgery” in its name, is not actually surgery; no scalpel or incision is used. This method can be likened to focusing weak sunlight from hundreds of different angles on a single spot with a magnifying glass and burning that spot. While each ray is harmless on its own, when they all converge on the AVM ball, they have a very powerful effect.
This high dose of radiation damages the walls of the vessels that form the AVM. This damage causes the vessels to gradually thicken and close over time, eventually turning into scar tissue. The most important feature of this process is that it is not instantaneous. It can take 2 to 3 years for the treatment to take full effect and for the AVM to completely close. During this waiting period, the patient continues to run the risk of bleeding.
This method is particularly ideal in the following situations:
- AVMs located in deep and sensitive areas of the brain where surgery would be very risky.
- AVMs smaller than 3 cm in size.
- Patients whose general health condition is not suitable for open brain surgery.
Radiosurgery gives the patient the chance to avoid the immediate risks of open surgery, but in return requires accepting a long waiting period with continued uncertainty and risk of bleeding. This is not only a medical but also a lifestyle decision.
What are the main differences between AVM disease treatment options?
Comparing these three main treatment modalities can help you better understand which pathway was chosen and why.
In terms of speed and accuracy, surgery is by far ahead. The problem is solved on the operating table and the risk of bleeding is immediately eliminated. Radiosurgery is at the other end of the spectrum; it is a slow but effective method that requires patience and takes years to produce results. Embolization usually acts as a bridge between the two, speeding up the process or making it safer.
In terms of risk and recovery time, the opposite is true. Open brain surgery inherently involves the highest immediate risk and the longest recovery period. The patient undergoes a recovery period that can last weeks or even months. Embolization and radiosurgery are much more comfortable. Patients can usually return to their normal lives after one day. However, the risk of bleeding during the long waiting period associated with radiosurgery is a burden in itself.
Ultimately, the choice depends on the answer to the question “immediately but with higher risk, or safer but waiting?”. This decision is made together, taking into account the nature of the AVM and the patient’s priorities.
What is the process and long-term expectations after AVM treatment?
Life after AVM treatment depends on the treatment and how successful it is. The prognosis for a patient whose AVM has been completely removed by surgery is usually excellent. Since the risk of bleeding is eliminated, the patient is expected to lead a normal life and have a normal life expectancy. After radiosurgery, the same favorable outcome is achieved when complete closure of the AVM is confirmed by angiography.
The recovery period after open surgery is the longest and most arduous. It may require weeks of fatigue and sometimes rehabilitation (physical therapy, speech therapy). Physical recovery is much faster after embolization and radiosurgery.
Whatever the treatment, the journey does not end with hospital discharge. Periodic MRI or angiography follow-up is required for many years to confirm that the AVM has completely disappeared and to make sure that there is no recurrence, which is very rare. Especially the comments and experiences of mall patients show how important it is to stick to this follow-up process.
So, what should mall patients pay attention to?
There are some points that are generally recommended in the post-treatment period:
- Never miss doctor appointments and follow-up imaging.
- Seek medical attention immediately for headaches, seizures or any new neurological symptoms.
- Avoiding strenuous activities such as heavy lifting, which can increase intracranial pressure, without a doctor’s approval.
- Keeping blood pressure under control and adopting a generally healthy lifestyle.
- In particular, patients who have had a hemorrhage and suffered permanent neurological damage (weakness, speech impairment, etc.) can apply for an AVM disability report to benefit from social and legal rights.
AVM can be a challenging process for both the patient and their family. However, when today’s advanced diagnostic and treatment methods are combined with a multidisciplinary approach, it is often possible to overcome this challenge and offer patients a healthy future.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.