Pacemaker removal becomes necessary when device infection, malfunction, or lead-related complications occur. Extraction is a delicate procedure requiring specialized techniques, as pacemaker leads are tightly attached to the heart and vessels.
Reasons for pacemaker removal include pocket infection, bloodstream infection, lead fractures, or device recalls. Early recognition of these issues is vital to prevent life-threatening complications such as sepsis or cardiac perforation.
The procedure can be performed through transvenous lead extraction using laser or mechanical sheaths. In high-risk cases, open-heart surgery may be required. Careful preoperative planning reduces procedural risks significantly.
Post-removal care involves infection control, close cardiac monitoring, and assessment for re-implantation if pacing is still necessary. Advanced technology allows safe re-insertion of newer devices, ensuring continued heart rhythm support when indicated.
| Medical Term | Pacemaker removal (Lead extraction) |
| Definition | Removal of the pacemaker and/or leads from the body |
| Main Causes | Device infection, electrode failure, vascular occlusion, device replacement, manufacturer recalls |
| Application Methods | Percutaneous (non-surgical) extraction, surgical (open heart) extraction |
| Techniques Used | Mechanical or laser sheath systems, catheter and lasso systems |
| Type of Anesthesia | Usually general anesthesia; in some cases local anesthesia |
| Process Sequence | Usually 1 to 3 hours; may take longer in complex cases |
| Complications | Risk of heart or vascular injury, bleeding, infection, arrhythmia, rarely death |
| Regeneration Process | Usually 1 to 2 days hospitalization; antibiotic treatment in case of infection and waiting period for new device implantation |
| Success Rate | Above average success rate in experienced centers |
| New Device Installation | In case of infection, the new device is usually inserted after a few days; in other cases it can be inserted in the same session |
Why Is Pacemaker Removal Necessary in Case of Infection?
The development of an infection in the pacemaker system is the most common and most urgent reason for removal of the device. In this case, the consensus of all international health authorities is that the pacemaker itself and all its wires should be completely removed, without exception. So why are strong antibiotics given intravenously not enough on their own?
The answer lies in the so-called “biofilm” that bacteria form to protect themselves. When bacteria adhere to the metal and plastic surfaces of batteries and their cables, they surround themselves with a sticky, slimy layer. You can think of this layer as an invisible fortress that the bacteria have built to protect themselves. This biofilm shield protects the bacteria from both your body’s immune cells and the most effective antibiotics we give intravenously. Antibiotics can clear free bacteria from your bloodstream, but they cannot destroy the main focus of infection that has infiltrated this fortress. Therefore, the only way to completely get rid of the infection is to physically remove and dispose of all this foreign material that the bacteria have made a home on, namely the battery and all its cables.
Infections associated with a pacemaker usually take two main forms. The first is local infection in the pocket area where the pacemaker is placed under the skin. Although this is called “local”, we assume that the whole system is infected and a full removal is still required.
Symptoms of local pocket infection are usually as follows:
- Redness
- Alik
- Increasing temperature in the region
- Pain or tenderness
- Purulent discharge from the wound site
- The device or cable piercing the skin and coming out (erosion)
The second and much more serious situation is when the infection enters the bloodstream (bacteremia) or spreads to structures inside the heart, such as the heart valves (endocarditis). This is a life-threatening emergency requiring immediate removal of the device.
Unfortunately, leaving an infected device in place and trying to continue treatment with antibiotics alone is extremely risky. Major scientific studies have shown that the risk of death in patients whose infected device is not removed is many times higher than in those whose device is removed. In fact, early removal within the first few days after diagnosis of infection has been shown to significantly increase the long-term survival rate. These data clearly show that pacemaker removal in the presence of infection is not an option but a life-saving necessity.
In which cases other than infection is pacemaker removal necessary?
Removal of a pacemaker is not always due to an infection. Sometimes it is done for reasons other than infection, such as malfunctioning wires, obstructions in the blood vessels or changing needs of the patient. In such cases, the decision is based on a careful risk-benefit analysis to determine what is the best and safest way forward for you, rather than an urgent imperative.
The main non-infectious causes of ablation are as follows:
- Cable (Lead) Failure
- Redundant or Recovered Cables
- Vascular Congestion
- Unmanageable Chronic Pain
- Interference with Other Medical Treatments
Cables are under constant stress of contraction and stretching over the years with every beat of your heart. Over time, this mechanical fatigue can lead to breaks in the cable or deterioration of its conductivity. In this case, the battery cannot properly stimulate the heart or detect the heart’s own rhythm properly, which can lead to serious problems such as fainting.
Sometimes the patient’s own heart function improves so much over time that the need for a battery is reduced or eliminated. Or, in rare cases, manufacturers may detect a problem with a particular series of cables and recommend replacing them for safety reasons.
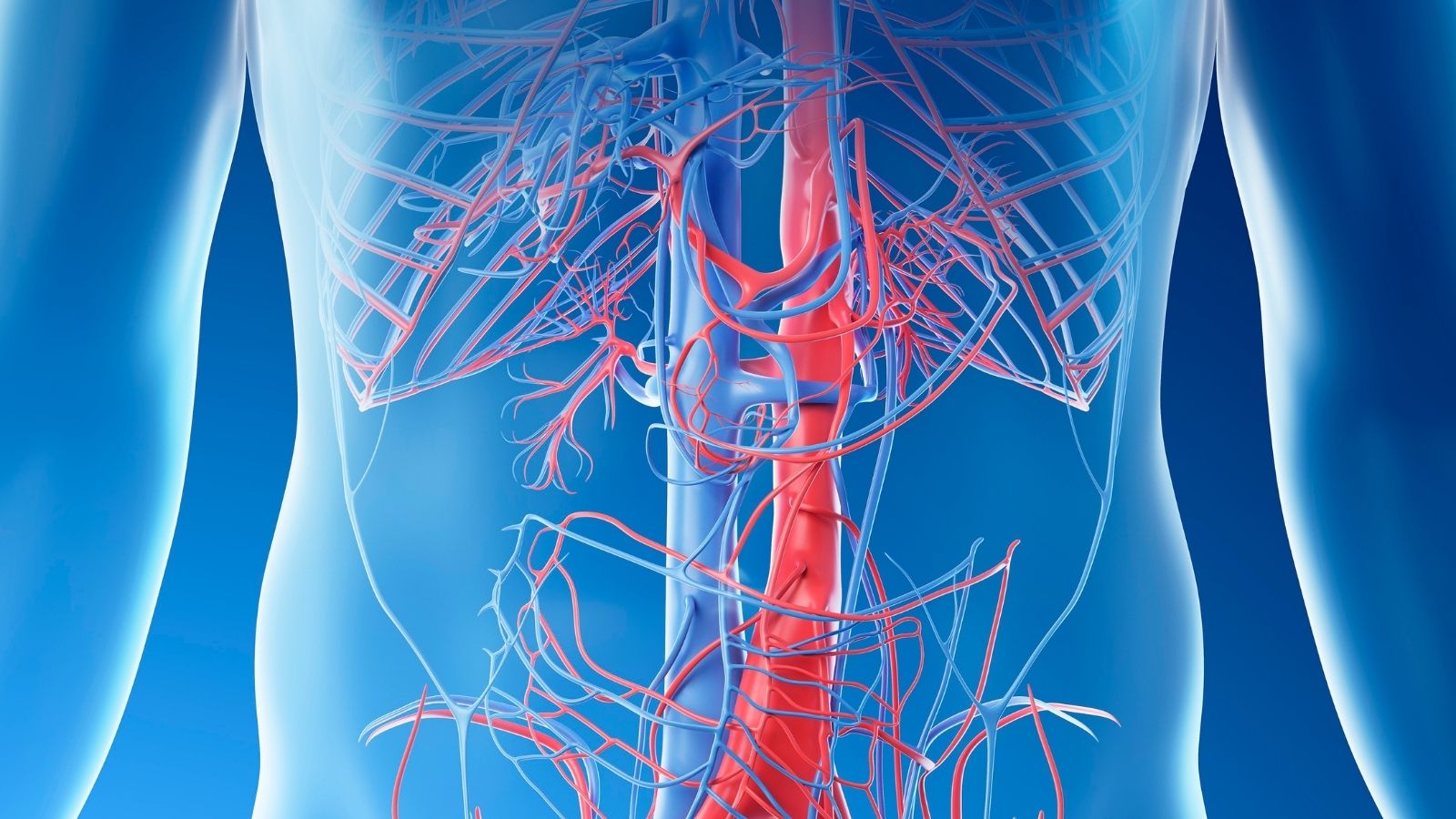
Scar tissue that forms around the cables over time can narrow or block the vein through which they pass. This is usually asymptomatic. However, if a new cable needs to be inserted from the same side or an existing battery needs to be replaced in the future, this obstruction can make access to the vein impossible. At this point, old and non-functional cables must be removed to make room for a new cable.
Rarely, there may be chronic, stabbing pain in the pocket area of the battery or along the cable trace that severely impairs the patient’s quality of life and does not respond to standard pain treatments. In addition, if another important medical procedure, such as radiotherapy for cancer treatment, is to be performed in the area where the battery is located, the device may need to be removed to avoid interfering with the treatment.
In such non-infectious situations, we are faced with two options: Remove the problematic cable completely, or leave it in place and add a new cable next to it? The latter option may seem simpler, but leaving a dysfunctional cable in the body carries potential risks in the future. “Abandoned” cables are more likely to become infected in the future and if they need to be removed years later, the procedure becomes much more difficult and risky. Therefore, especially in younger patients, it is often a safer and more accurate long-term strategy to have the problematic cable removed at an experienced center to prevent potential future problems in the first place.
How Do They Prepare for Pacemaker Removal Surgery?
Pacemaker removal is a complex procedure that requires care and attention. For this reason, we carry out a meticulous preparation and planning process before entering the operating room. You can liken this process to a detailed map study before an important journey. Our goal is to anticipate all potential obstacles on the road, minimize risks and determine the safest route for you.
This rigorous preparation and evaluation process includes the following steps:
- Comprehensive Medical Evaluation
- Detailed Device Inquiry
- Blood Tests
- Advanced Imaging Studies
- Multidisciplinary Team Meeting
First of all, any other medical conditions you have, such as diabetes, chronic kidney disease, etc., are carefully examined. Because these conditions can affect both your risk during the procedure and the speed of your recovery after surgery. Then, just before surgery, your pacemaker will be interrogated in detail with a special programming device. The most vital purpose of this interrogation is to determine how “dependent” your heart is on the pacemaker. If your heart cannot beat safely and at a sufficient rate without battery support, we call this condition “battery dependency”. For these patients, a temporary pacemaker solution is planned in advance to secure the heart rhythm during and immediately after the removal procedure.
Standard blood tests check your kidney function, blood count and basic parameters such as your blood clotting ability. The most important part of our map is the imaging studies. These tests allow us to understand the number of cables, their type, their exact position inside the heart and, most importantly, the degree of adhesion with the surrounding tissues. We usually start with a visual roentgenogram. Then, a “transesophageal echocardiogram” (TEE), especially through the esophagus, gives us a much clearer view of the inside of your heart and its valves. This test is the gold standard for detecting infection clumps on the wires. In particularly complex cases, we may also order a computed tomography (CT) scan to make a three-dimensional map of the veins and cables. It shows where and how tightly these cables are attached to the vessel wall, helping the surgeon to determine the surgical strategy.
Finally, this decision and planning is done jointly by a team of specialists, not by a single physician. This team includes the cardiovascular surgeon who will perform the procedure, an anesthesiologist, an infectious disease specialist and experienced operating room staff. This teamwork is indispensable for your safety.
What Modern Methods Are Used for Pacemaker Removal?
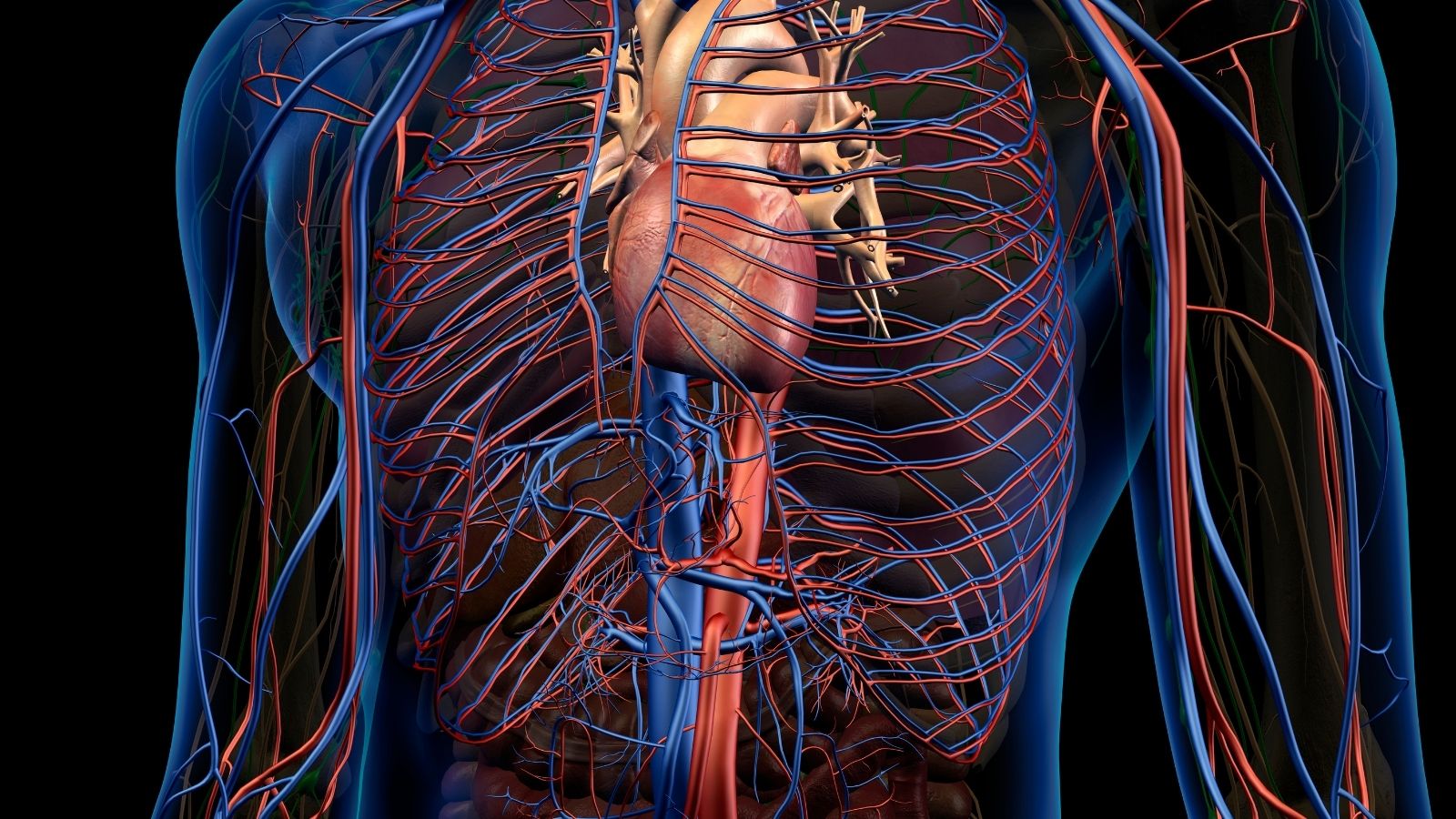
Modern pacemaker removal is a minimally invasive procedure that is performed without opening the chest cage, usually at the site of the original pacemaker insertion, usually below the shoulder. Due to the high potential for risk, this procedure is only performed by surgeons with specialized training and high case experience in fully equipped hybrid operating rooms with the possibility of emergency open heart surgery. General anesthesia is generally preferred for patient comfort and procedure safety.
The most technically challenging part of this procedure is the hard and adhesive scar (fibrotic) tissue that the body has built up around the cables over the years. The longer a cable stays in the body, the thicker this scar tissue becomes, cementing it to the vessel walls and heart muscle. Our goal is to release the cable by opening these adhesions in a very controlled and gentle way, without the slightest damage to the heart or the vessel.
For this, as surgeons, we follow a “toolbox” approach. That is, we start with the simplest tool and move on to more complex and high-tech tools as needed. This is a delicate step-by-step process. First a gentle pulling force is applied to the cable, but this usually only works with very newly installed cables.
In many cases, we stabilize the cable by using a thin wire called a “locking stylet” which we run from the inside of the cable to the end. This ensures that the pulling force is transmitted directly to the sticky end. If this is not enough, the real surgery begins. A hollow tube called a “sheath” is placed over the cable, which acts as a rail for it. The surgeon advances this sheath slowly, mechanically stripping the scar tissue with its tip and removing adhesions.
If the scar tissue is very old, hard and frayed, where mechanical force is insufficient, “power-assisted” sleeves come into play. These are high-tech tools that allow us to move confidently through even the toughest adhesions. There are two main types of these advanced sheaths:
- Laser Energized Sheaths
- Rotational Sheaths
The laser sheath generates controlled laser energy through fiber optic fibers at its tip, “vaporizing” the scar tissue without radiating heat to surrounding tissues. The rotary-headed sheath, on the other hand, mechanically pierces or cuts through even the hardest and most fragmented tissues with a miniature cutting mechanism at its tip. Which instrument to use is determined by the surgeon based on the structure of the scar tissue and the patient’s anatomy.
Sometimes, the standard approach through the shoulder region is unsuccessful. In these rare cases, we grasp the cable from below with special tools like a “lasso”, entering through the large veins in the groin or neck. This “rescue” maneuver ensures successful completion of the operation, even in the most difficult cases.
What is the Success Rate of Pacemaker Removal?
We understand that you have concerns about this, but with modern techniques and in experienced hands, the results of this procedure are extremely gratifying. Transvenous pacemaker removal is a highly successful procedure when performed in specialized centers with a high number of cases. According to large international records and our own experience, more than one to two percent of the targeted cables are completely and safely removed from the body.
We assess success in two different ways. The first is “radiologic success”, in which all targeted cable fragments, including the smallest, are completely removed from the body. The second is “clinical success”, in which enough cable material is removed to eliminate the reason for performing the procedure (e.g. to treat infection), leaving behind a very small, clinically insignificant fragment. In both definitions, the success rates are above . These high rates provide strong evidence of the effectiveness and reliability of the procedure.
What are the Possible Risks of Pacemaker Removal?
As with any surgical intervention, pacemaker removal has potential risks. While it is generally a safe procedure, it is not a zero-risk procedure. Transparently discussing these risks is essential for patient safety and informed consent. Even in the most experienced hands, complications can occur, albeit at a low rate.
The most worrisome and serious complication is rupture of the main vein (superior vena cava) to which the cables are attached or, rarely, the heart wall. This can lead to internal bleeding in the chest that requires urgent intervention. This is why the procedure is always performed in a fully equipped operating room, with a team of cardiac surgeons standing by. Fortunately, such major complications are rare, occurring in about 1-2% of cases. The risk to life from the procedure is very low and is usually reported to be between 2 and 5 per thousand.
In addition, there may be minor complications, such as bleeding in the battery pocket (hematoma), a collapsed lung (pneumothorax) or slight damage to the heart valve, which are less serious and can usually be managed successfully.
Some factors have been identified that may slightly increase the risk of complications:
- The patient is female (usually due to more delicate vascular structures)
- The patient has comorbidities such as chronic renal failure
- Emergency extraction procedures due to infection
- The length of time the cable remains in the body is too long (one of the most important factors)
- Removing three or more cables at the same time
The presence of these risk factors requires us to plan the procedure more carefully. However, it should be remembered that the most important factor that affects the outcome and is under the patient’s control is to perform the procedure in a “high-volume” center with high case experience. It has been scientifically proven that complication rates are significantly lower in experienced centers.
What is the recovery process after pacemaker removal?
Pacemaker removal is not a process that ends when the surgery is over. The post-operative period is just as critical as the surgery itself, especially in cases of infection. This period is aimed at your safe recovery and, if necessary, a smooth transition to a new device.
Immediately after the procedure, your vital signs will be closely monitored for several hours in a recovery room or intensive care unit. You will usually need to stay in hospital for at least one night. During this time, a follow-up chest X-ray and ultrasound of the heart (echocardiography) are performed to confirm that there are no problems.
When you are discharged, you will be told in detail what to take care of at home. Care of the wound site and activity restrictions are particularly important. In general, these are the rules you must follow:
- Avoiding overuse of the arm on the operated side
- Not raising the arm above shoulder level
- No sudden and forceful movements
- Not lifting objects heavier than 5 kilograms for a certain period of time (usually 4-6 weeks)
These restrictions are vital both for the healthy healing of your wound site and, if a new device has been installed, to ensure that its cables are securely in place and fixed.
When is a new device implanted after pacemaker removal due to infection?
This is one of the most common and most worrying questions asked by patients whose pacemaker has been removed due to infection. To completely eliminate the risk of the infection recurring in the body, the insertion of a new pacemaker is deliberately delayed for a while. This is the most important measure for your health.
International guidelines recommend that before fitting a new device, we should see that your blood cultures have been completely clear for at least 72 hours under antibiotic treatment. If there is a serious infection that has spread to the heart valves (endocarditis), this waiting period is usually extended to at least 14 days.
So how can a patient whose heart depends on a pacemaker safely go through this waiting period? For these patients, we implant a “temporary pacemaker” to keep the heart beating safely. This temporary system provides you with a reliable heart rhythm while you receive your infection treatment and wait for your body to be completely cleansed, allowing you to get through this process safely.
Once the infection has been proven to be completely cured, the new permanent device is almost always attached to the opposite side of the body to avoid the infected area. This holistic and careful approach aims not only to solve the current problem, but also to safeguard your future health.
Frequently Asked Questions
Why is a pacemaker removed?
A pacemaker can be removed in cases such as infection, device malfunction, electrode problems, expired battery life or no longer needed for treatment.
Is pacemaker removal difficult?
In simple cases, removal is easy, but in batteries that have been in the body for a long time, the procedure can be more complicated because the electrodes adhere to the vessel wall.
How is pacemaker removal performed?
The battery and electrodes are removed with special equipment, usually under local or general anesthesia. In some cases, surgery may be necessary.
What happens after a pacemaker is removed?
If the patient’s heart rhythm needs to continue to be controlled by the battery, a new battery is inserted. If not, the patient is monitored.
How long does it take to remove a pacemaker?
The processing time can vary from 1 to 3 hours depending on the complexity of the situation.
Is pacemaker removal dangerous?
Like any surgical procedure, it carries some risks. Complications such as bleeding and vascular injury may occur, especially during removal of infected electrodes.
In which cases is pacemaker removal urgent?
Spread of infection (sepsis), severe battery failure or systemic reactions may require emergency removal.
Is there a risk of infection after pacemaker removal?
If the infected battery has been removed, antibiotic treatment is given to clear any remaining infection. The risk is lower for those who are clean.
Can a pacemaker be reinserted in the same place after it has been removed?
Often a different site is preferred, especially if there is an infection, a battery is placed on the opposite side.
Who does pacemaker removal?
This procedure is usually performed by cardiologists or cardiovascular surgeons who specialize in electrophysiology.
Will the patient whose pacemaker is removed remain in intensive care?
Follow-up after the procedure depends on the general condition of the patient. If there is no risk of complications, you are usually discharged soon.
Can a patient who has had a pacemaker removed have a temporary battery?
Yes, in some cases a temporary pacemaker can be implanted to keep the heart’s rhythm under control.
Can the patient return to normal life after pacemaker removal?
If a new battery is installed or the arrhythmia is under control, daily life can be resumed within a few days.
Is pacemaker removal covered by the SSI?
Yes, SSI and private insurances usually cover this procedure when there is an indication for it.
Can problems occur again after a pacemaker is removed?
Rhythm disturbances may recur depending on the underlying heart disease. Regular follow-up is important.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.