Aortic dissection is a life-threatening condition where a tear occurs in the aortic wall, allowing blood to flow between its layers. This disrupts circulation and can rapidly lead to organ damage or rupture, requiring immediate medical intervention.
Symptoms of aortic dissection typically include sudden, severe chest or back pain, fainting, shortness of breath, and neurological deficits. Risk factors include hypertension, connective tissue disorders, and a history of cardiovascular disease.
Diagnosis is confirmed through imaging methods such as CT angiography, echocardiography, or MRI. Emergency treatment may involve blood pressure control, pain management, and urgent surgery to repair or replace the affected aortic segment.
Long-term management focuses on strict blood pressure regulation, lifelong cardiology follow-up, and lifestyle modifications. Patients who survive an aortic dissection require regular imaging and medical supervision to prevent recurrence or complications.
| Medical Name | Aortic Dissection |
| Type | Acute vascular disease |
| Affected System | Cardiovascular system |
| Prevalence | Rare but deadly |
| Causes | Hypertension, connective tissue diseases (Marfan syndrome, Ehlers-Danlos), trauma, aortic aneurysm |
| Symptoms | Sudden and severe chest or back pain, fainting, shortness of breath, symptoms of stroke, low blood pressure |
| Diagnostic Methods | Computed tomography (CT) angiography, Transesophageal ECHO, Magnetic Resonance (MR) angiography |
| Treatment Methods | Type A: Emergency surgery; Type B: Medical treatment (antihypertensive) and endovascular intervention when necessary |
| Complications | Aortic rupture, organ ischemia, stroke, cardiac tamponade, death |
| Monitoring | Strict blood pressure control, regular imaging (CT/MR), lifelong follow-up |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is Aortic Dissection and What Happens in the Vessel Wall?
To better visualize aortic dissection, think of the aorta as the main water pipe in our home. This huge pipe, which carries clean blood pumped from our heart to the most remote corners of our body, is designed to withstand enormous pressure. Its wall is made up of three sturdy interwoven layers. The innermost layer is smooth and allows blood to flow freely. It is the middle layer, rich in muscle and elastic fibers, that provides the real strength and flexibility. The outermost layer is like a protective sheath.
Aortic dissection usually begins with a small fray or tear in the inner layer of this structure, which has weakened over the years. The high-pressure blood generated by each beat of the heart finds this weak spot and, like a knife, seeps between the layers of the vessel wall. This tears the structure of the vessel into layers, like an onion. The blood opens a new, abnormal pathway (“false lumen”) alongside the main pathway through which it should normally flow (“true lumen”).
This has two major dangers. First, the blood pressure inside this newly formed false duct can squeeze the original duct from the outside and narrow it. This compression can block blood flow to the smaller vessels that branch off from the aorta and supply vital organs such as the brain, heart, kidneys and intestines. We call this condition “malperfusion” and it is the main cause of serious consequences such as strokes and heart attacks. The second and most frightening danger is that blood pressure can tear through the weak outer wall, which is now reduced to a single layer. This is called a “rupture” and means that blood can leak into the chest or abdominal cavity, causing fatal internal bleeding within minutes. This is why aortic dissection is a race against time.
What Are the Main Causes and Risk Factors for Aortic Dissection?
Aortic dissection is not something that usually happens “out of the blue”. It is caused by a number of causes and risk factors that silently weaken the aortic wall over the years. Knowing these factors is critical for both prevention and early diagnosis.
The most important chronic conditions that decrease the resistance of the aortic wall and increase the risk of dissection are:
- High blood pressure (Hypertension)
- Arteriosclerosis (Atherosclerosis)
- Pre-existing aortic aneurysm
Among these factors, uncontrolled high blood pressure is by far the most common and most important cause. Three quarters of patients have a history of high blood pressure. The constant high pressure acts like a continuous hammer blow on the aortic wall, causing it to wear and harden over time.
Some people are more prone to this disease because of congenital structural defects or genetic inheritance. Risk factors in this group are as follows:
- Marfan syndrome
- Loeys-Dietz syndrome
- Ehlers-Danlos syndrome (Vascular type)
- Bicuspid aortic valve
- Family history of aortic disease
In particular, connective tissue diseases, such as Marfan’s, defect the basic building materials (elastin and collagen) that make up the aortic wall. This makes the vessel weaker, more flexible and prone to tearing. A congenital two-leaflet aortic valve (bicuspid aortic valve), which should normally have three leaflets, leads to abnormal blood flow and stress at the beginning of the aorta, increasing the risk of dissection.
Lifestyle and certain other conditions can also affect the risk. Factors in this group are:
- Advanced age
- Male gender
- Cocaine or amphetamine use
- Intense and demanding weight lifting
- Severe blows to the chest area (such as a traffic accident)
- Pregnancy (rarely, especially if there is an underlying connective tissue disease)
What are the Most Common Symptoms of Aortic Dissection?
Aortic dissection often presents itself with very sudden and dramatic symptoms. Recognizing these symptoms can be life-saving. Almost all patients report a sudden and very severe onset of symptoms.
The most classic and warning signs of aortic dissection are the following:
- Sudden onset, very severe chest or back pain
- Pain character described as tearing, ripping or stabbing
- Pain of a wandering nature (radiating from the chest to the back, neck or abdomen)
- Sudden loss of consciousness or fainting (syncope)
- Cold sweating and pallor
- Severe shortness of breath
This pain is often described by patients as “the worst pain I have ever felt in my life”. It does not gradually increase like the pain of a heart attack; it reaches its peak as soon as it starts. Migratory pain (migratory pain), in which the pain is displaced in parallel with the progression of the dissection along the aorta, is a very typical finding.
When a dissection disrupts the blood supply to organs, symptoms specific to that organ also appear. This is an indication of how wide an area the dissection has affected. Other important signs to look out for are as follows:
- Stroke-like symptoms (facial shift, slurred speech, weakness in the arm or leg)
- Heart attack-like chest pain
- Weak or absent pulse in one arm compared to the other
- Significant difference in blood pressure measured between the two arms (usually more than 20 mmHg)
- Severe abdominal pain
- Sudden onset of severe pain, coldness, pallor or paralysis in the legs
Sometimes, especially in elderly patients, the dissection can also be painless and only present with a sudden fainting, paralysis or shortness of breath. These “silent” dissections are even more dangerous as they can cause delays in diagnosis.
How Is Aortic Dissection Classified and Why Is It Vital?
When an aortic dissection is diagnosed, the first thing physicians do is to determine which area of the aorta is affected by the tear. This is the most critical information that directly affects the patient’s treatment plan and chances of survival. For this purpose, the globally recognized Stanford Classification is used. This classification provides a roadmap that determines the urgency of treatment.
This simple and practical classification divides dissection into two main types:
- Stanford Tip A
- Stanford Tip B
In a Stanford Type A dissection, the tear affects the ascending aorta (ascending aorta), which comes out of the heart and includes the aortic arch. This is the most dangerous and urgent type. This is because the coronary arteries supplying the heart, the aortic valve and the main vessels carrying blood to the brain leave from this area. When the tear affects these structures, it can lead to fatal consequences such as heart attack, heart failure or stroke. The diagnosis of Type A aortic dissection is therefore considered an absolute surgical emergency and the patient is immediately prepared for surgery.
In a Stanford Type B dissection, the tear is in the descending aorta (descending aorta) after the origin of the left arm vessel and does not involve the ascending aorta close to the heart. This type usually poses a less immediate threat than Type A. Unless complications develop, it can initially be managed with medication in intensive care. However, this does not mean that the danger has passed. If a Type B dissection disrupts the blood supply to the organ or there is a risk of rupture, it too becomes a situation requiring urgent intervention.
Which methods are used to diagnose aortic dissection?
Aortic dissection is also known as the “great imitator” because its symptoms can be confused with many other diseases (especially heart attacks). The diagnostic process begins with the physician’s suspicion based on the patient’s typical history (sudden, tearing pain) and examination findings (such as the difference in blood pressure between the two arms).
In the presence of this strong clinical suspicion, modern technologies that image the aorta in detail are used to confirm the diagnosis and plan treatment. The gold standard imaging methods used in the diagnosis are as follows:
- Computed Tomography Angiography (CTA)
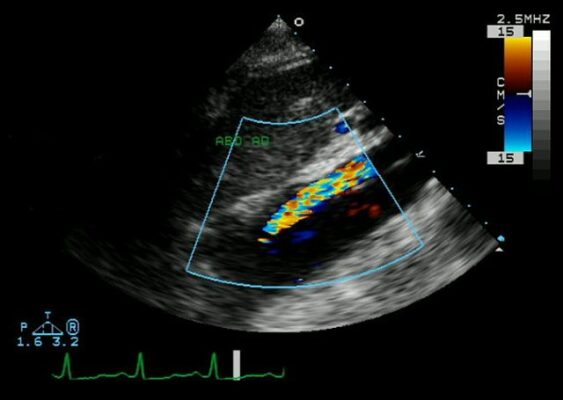
- Transesophageal Echocardiography (TEE)
- Magnetic Resonance Angiography (MRA)
Computed Tomography Angiography (CTA) is a fast and highly reliable procedure that is most commonly used in emergencies today. A series of X-ray images are taken very quickly while a contrast agent (a dye) is injected into the patient’s vein. The computer combines these images to produce a detailed three-dimensional map of the aorta and all its branches. CTA shows the presence, type and extent of dissection with an accuracy close to 0.
Transesophageal Echocardiography (TEE) is invaluable, especially for critically ill patients who cannot be transported to CT scan. A flexible tube with a small ultrasound probe at the end is lowered through the mouth into the esophagus. Because the esophagus is so close to the heart and aorta, this method provides very clear, real-time images of the aorta and heart. Its biggest advantages are that it is radiation-free and can be performed at the bedside.
Magnetic Resonance Angiography (MRA) is another valuable imaging modality that does not involve radiation. It offers excellent soft tissue resolution. However, its use in emergency situations is limited due to the long acquisition time. It is generally preferred in stable patients or for long-term follow-up of chronic dissections.
How is Type A Aortic Dissection Treated?
Once a Stanford Type A aortic dissection is diagnosed, the race against time begins. This is an absolute surgical emergency with a mortality rate of P in the first 48 hours if left untreated. Therefore, the only and undisputed treatment option is emergency open heart surgery.
During the preparations for surgery, the patient is kept in intensive care. The aim is to reduce the stress on the aortic wall by lowering blood pressure and heart rate with aggressive drug therapy and to slow the progression of the tear until surgery.
The main goal of the operation is to completely remove the main entrance tear where the dissection started and the diseased ascending aortic segment. In its place, a tube graft (artificial vessel) made of a special, durable synthetic material such as Dacron is sutured. This procedure is an open-heart surgery in which the sternum is cut and requires the use of a heart-lung machine. If the dissection has damaged the aortic valve, the valve is repaired or replaced during this operation.
Type A aortic dissection operations are among the most complex and challenging operations in cardiovascular surgery. Therefore, performing such surgeries in specialized centers with high case volumes, experienced surgeons and multidisciplinary aortic teams (cardiologists, radiologists, anesthesiologists) significantly increases the patient’s chances of survival and a successful outcome.
Which Approaches are Followed in the Treatment of Type B Aortic Dissection?
In contrast to Type A dissection, the treatment approach for Type B dissection is determined by whether the patient’s condition is “complicated” or not.
Uncomplicated Type B Dissection: This condition is considered “uncomplicated” if the patient’s general condition is good, there is no problem with blood flow to the organs and the pain can be controlled with medication. The gold standard treatment for these patients is optimal medical therapy. The patient is closely monitored in the intensive care unit. Stress on the aortic wall is minimized with aggressive medication to lower blood pressure and heart rate and strong painkillers.
Complicated Type B Dissection: The presence of one of the following conditions “complicates” the dissection and necessitates emergency intervention:
- Rupture (rupture or threat of rupture of the aorta)
- Malperfusion (impaired blood supply to organs such as kidneys, intestines, legs)
- Severe pain that cannot be controlled despite medication
- High blood pressure that cannot be controlled with medication
- Rapid and dangerous increase in aortic diameter during follow-up
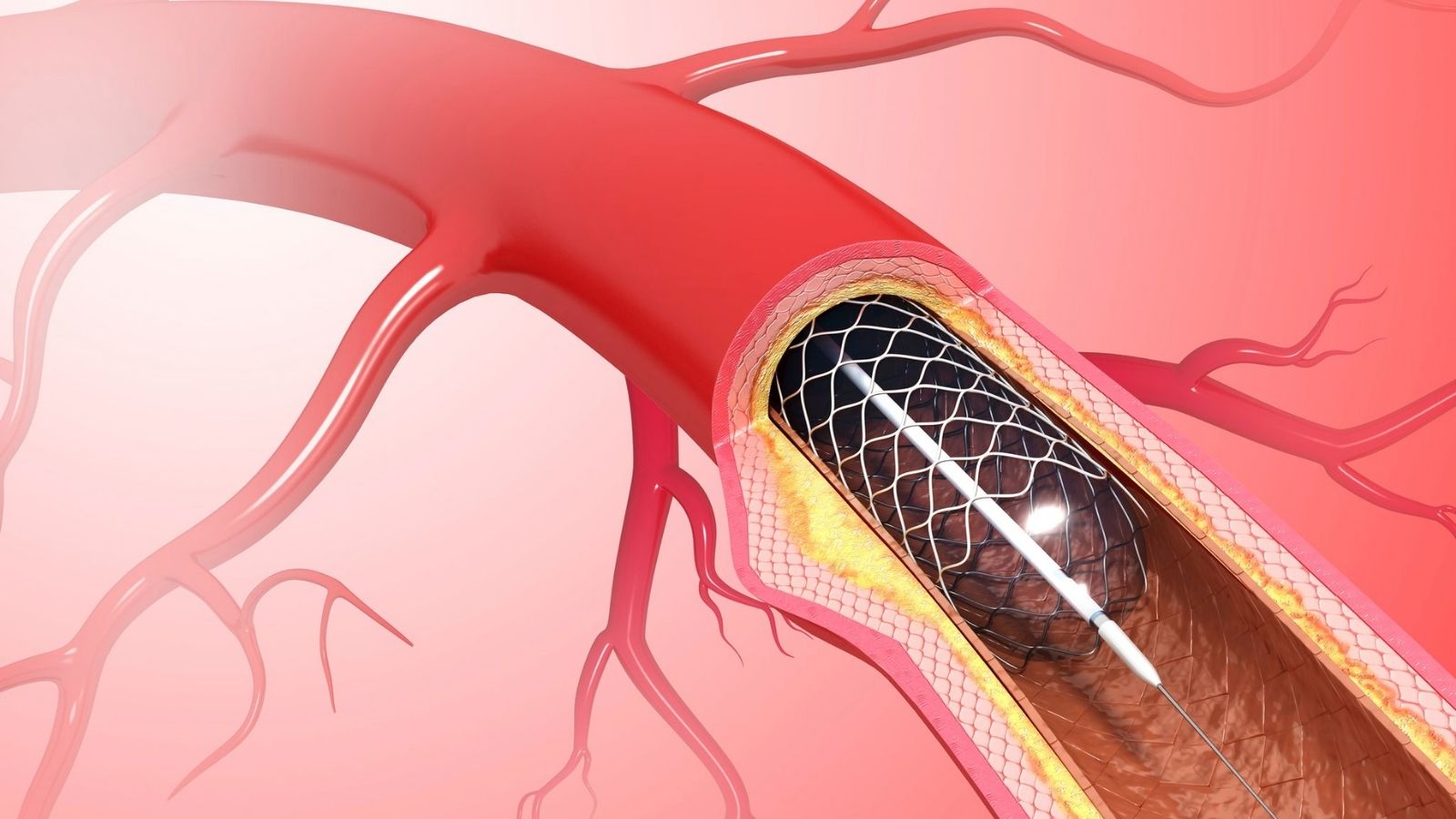
In these complicated cases, the treatment option today is usually a minimally invasive procedure called Thoracic Endovascular Aortic Repair (TEVAR). Unlike open surgery, TEVAR is performed through a small incision in the groin artery. Through this incision, a delivery system containing a metal skeleton (stent-graft) with a fabric-covered tip is advanced into the aorta under X-ray visualization. The stent-graft is deployed to close the main tear from the inside through which blood leaks into the vessel wall. This redirects blood flow to the main channel where it should be, improving organ blood supply and eliminating the risk of aortic rupture.
What is the Recovery Process After Aortic Dissection Surgery?
| Recovery Time | It may take about 4-6 weeks, depending on age, general health and the location of the dissection. |
| Physical Activity | Light exercise is recommended for the first 6-8 weeks; heavy lifting should be avoided. Long-term regular, gentle exercise is encouraged. |
| Blood Pressure Control | It is the most critical factor; target blood pressure should generally be kept below 140/80 mmHg. |
| Medication Use | Beta blockers, ACE inhibitors and other antihypertensive drugs may be needed for life. |
| Nutrition | A low sodium, low cholesterol, high fiber and balanced diet is recommended. |
| Psychological Status | Depression and anxiety may occur after a life-threatening situation; psychological support is beneficial. |
| Imaging Follow-up | Regular CT angiography or MRI monitoring of the aorta is necessary; at least once a year. |
| Complications | There are risks such as re-dissection, aneurysm development, problems at the prosthesis site. |
| Work and Social Life | Work that does not require physical exertion can be returned to with the doctor’s approval; usually after 2-3 months. |
| Sexual Activity | It is usually possible after 4-6 weeks, with the approval of the doctor, after blood pressure control is achieved. |
| Smoking and Alcohol | Strictly prohibited; poses a serious risk to vascular health. |
| Vehicle Use | it can be started after 4-6 weeks, when concentration and physical ability are restored. |
Recovery from major surgery for aortic dissection is a process that requires patience and care. This process involves not only physical but also psychological recovery.
Patients usually stay in intensive care for a few days after surgery and in hospital for 1-2 weeks in total. For the first few months after discharge, the focus is on allowing the body to repair itself. It is normal to feel tired and weak during this period. There are some basic restrictions that must be followed during the first period of recovery:
- Avoidance of driving (usually 4-6 weeks)
- not lifting objects weighing more than 5 kilograms
- Avoid pushing or pulling heavy objects
- Protecting the sternum from impacts
Experiencing such a sudden life-threatening event can have a serious psychological impact on patients. Post-traumatic stress disorder, anxiety, depression and living with the fear that dissection may occur again at any time are common. Therefore, the psychological aspect of the healing process should not be ignored and professional support or patient support groups should be sought if necessary. Remember that you are not alone in this journey.
What Lifelong Changes Are Required After Aortic Dissection?
Aortic dissection becomes a “chronic” disease after the acute phase is over. This means that the patient cannot say “I’m cured and it’s over”, but enters a lifelong process of follow-up and management. The long-term success of treatment depends on the patient taking an active role in managing their own health.
Blood Pressure Control: This is the most critical and indispensable rule. Blood pressure should be strictly controlled throughout life, usually with a BP below 120-130 mmHg. This requires taking medication regularly every day and monitoring blood pressure at home.
Heart Friendly Diet: Reviewing your eating habits is one of the best things you can do for your aortic health. The basic principle is to adopt a diet that will help keep blood pressure and cholesterol under control.
Here are some points to consider in your diet:
- Reducing salt and sodium
- Avoid saturated and trans fats (red meat, butter, processed snacks)
- Limit processed foods and sugary drinks
- Consume plenty of fresh vegetables and fruits
- Choosing whole grains instead of white bread
- Choosing healthy protein sources (fish, skinless chicken, legumes)
Physical Activity and Exercise: A sedentary life is strongly discouraged. Regular and moderate exercise is beneficial for both your physical and mental health. But balance is very important here.
Safe exercises you can do include:
- Brisk walking
- Swimming
- Cycling (light to moderate pace)
- Multi-repetition resistance exercises with light weights
- Activities that increase blood pressure suddenly and excessively should be avoided.
Activities to avoid are as follows:
- Heavy weightlifting and intensive weight lifting
- Movements that require pushing while holding your breath (Valsalva maneuver)
- Sports that require explosive power such as sprinting and jumping
- Competitive and contact sports (such as soccer, basketball, wrestling)
Lifelong follow-up: This is one of the most important issues. You need a lifetime of regular medical check-ups and imaging (annual CTA or MRA) to monitor the rest of your aorta and detect possible late complications (such as the development of a new aneurysm) at an early stage. Keeping up with these checks is the only way to prevent a future disaster.
Familial Screening Finally, it is strongly recommended that first-degree relatives (mother, father, siblings, children) of a person with aortic dissection be evaluated by a cardiovascular surgeon and screened with an echocardiogram, as they may also have a genetic predisposition.
Frequently Asked Questions
What is the mortality rate of aortic dissection?
Especially in dissections affecting the artery coming out of the heart (Type A), if left untreated, the risk of death in the first 48 hours increases every hour and the rate of death before reaching the hospital is high. However, with early diagnosis and emergency surgery, the success rate is currently high. Early diagnosis saves lives.
How long does a ruptured aortic artery live?
Aortic dissection is a very urgent condition where even seconds count. If the artery coming out of the heart ruptures, life is limited to hours without immediate intervention. In other parts of the body, time can sometimes be bought with medication. “Waiting” is not an option; urgent intervention is essential.
How many hours does aortic dissection surgery take?
Aortic dissection surgery is a complex and major operation. It usually takes 4 to 8 hours, sometimes longer, depending on the location and extent of the tear. It is performed with a heart-lung machine and advanced technologies.
Does aortic dissection show up on ECG?
ECG does not show dissection directly. Dissection can sometimes mimic a heart attack and there may be signs of a crisis on the ECG. Advanced imaging modalities such as computed tomography (CT angiography) are required for definitive diagnosis.
What are the clinical signs of aortic dissection?
The most typical symptom is sudden onset of very severe chest and back pain with a tearing pain. The pain may change location. Loss of pulse in the arms and legs, blood pressure difference, loss of consciousness, stroke-like symptoms and hoarseness may be observed. All require urgent intervention.
Is aspirin used in aortic dissection?
Absolutely not! Aspirin and similar blood thinners increase bleeding and can be fatal, as the vessel wall is torn in a dissection. Do not self-medicate in case of sudden chest pain, consult a doctor immediately.
What is the difference between aortic aneurysm and dissection?
An aneurysm is a balloon-like enlargement of the aorta and usually grows slowly. A dissection is when the vessel wall suddenly ruptures and blood leaks between the layers of the wall. Not all aneurysms rupture, but most dissections have a weak vessel wall underneath.
Is troponin elevated in aortic dissection?
It can rise. If the tear affects the heart vessels, a heart attack develops and troponin rises. This can make diagnosis difficult. Therefore, it is important not to focus only on heart attacks when troponin is elevated.
What should we do to protect the aorta?
Keep blood pressure under control, quit smoking, eat a healthy Mediterranean-type diet and walk regularly. If you have a family history or are at risk, have regular check-ups with a cardiovascular surgeon even if you have no complaints. Early prevention saves lives.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.