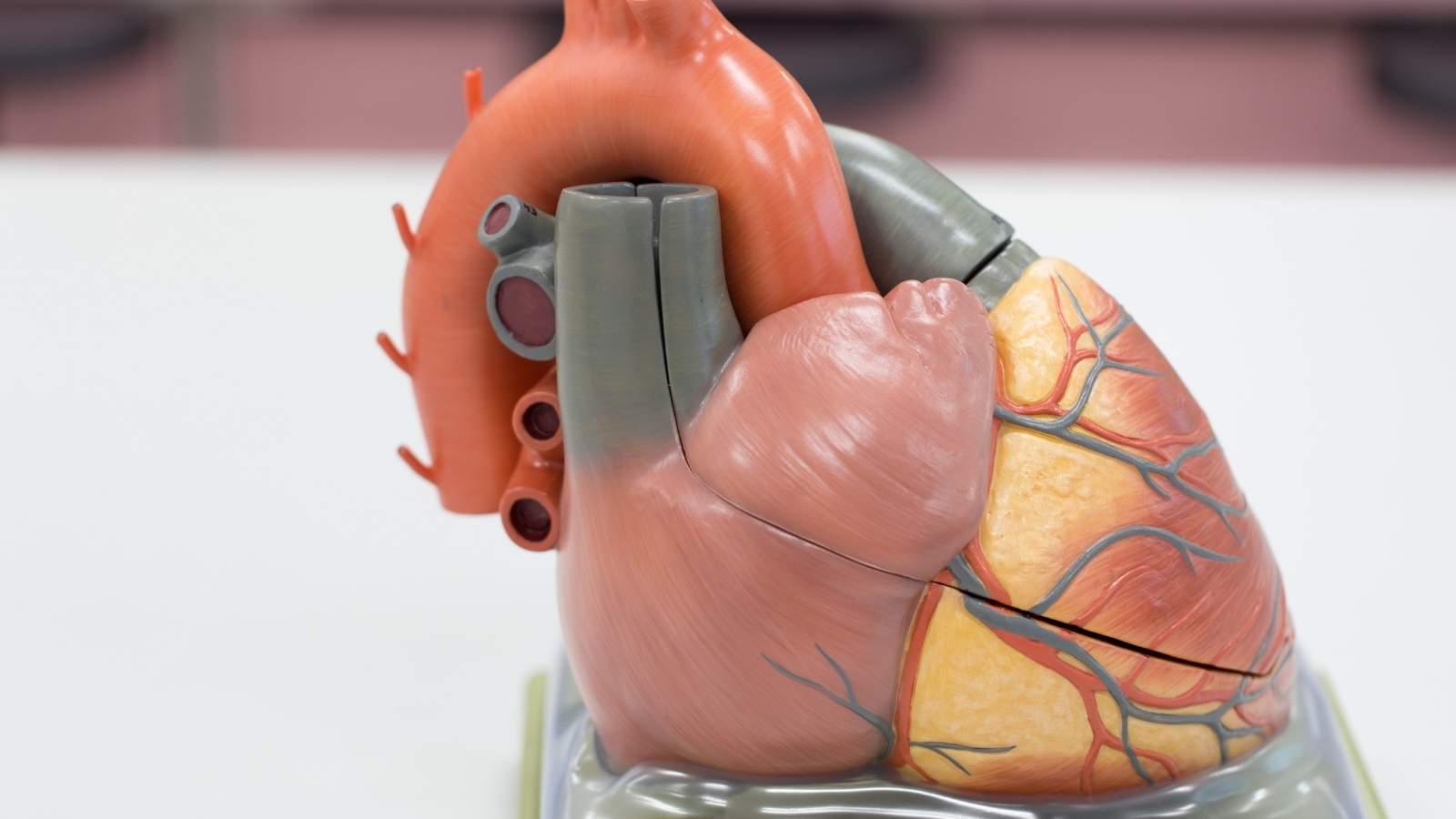
Atrial myxoma is the most common type of primary cardiac tumor, typically located in the left atrium. It can obstruct blood flow, cause embolic events, or mimic valvular heart disease, making early diagnosis and surgical removal essential for preventing life-threatening complications.
Symptoms of atrial myxoma vary depending on tumor size and location, often presenting as shortness of breath, fainting, or palpitations. Embolic complications may lead to stroke or peripheral arterial occlusion, underscoring the importance of recognizing warning signs promptly.
Diagnosis of myxoma relies on advanced imaging techniques such as echocardiography, MRI, and CT. Echocardiography, in particular, allows real-time visualization of the tumor’s size, mobility, and attachment site, playing a critical role in both initial assessment and follow-up.
Treatment involves complete surgical excision, which generally results in excellent long-term outcomes. Recurrence is rare but possible, especially in familial syndromes like Carney complex. Lifelong clinical follow-up is recommended to detect any recurrence or late complications.
| Definition | Benign primary tumor of the heart, usually located in the left atrium (atrium) |
| Causes | Usually the cause is unknown; rarely it may be genetic (familial myxoma syndromes) |
| Risk Factors | Middle age, female gender, family history of myxoma (rare) |
| Symptoms | Shortness of breath, palpitations, fainting, chest pain, weakness, fever, weight loss, embolism (clotting) symptoms |
| Diagnostic Methods | Echocardiography (the most important diagnostic method), ECG, CT or MRI, cardiac catheterization |
| Treatment Methods | Surgical removal of the entire tumor (only treatment method) |
| Complications | Embolism (clots in organs such as the brain, kidneys, legs), valve obstruction, arrhythmias, sudden death |
| Improvement and Follow-up | Regular postoperative echocardiography controls, monitoring the risk of nux |
| Prevention Methods | No specific prevention; regular cardiologic control is recommended if there is a family history |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is Cardiac Myxoma and why is it a danger?
In its simplest definition, a cardiac myxoma is a benign tumor that grows inside the heart. the word “benign” is usually reassuring because it means that it has not spread throughout the body, like cancerous cells, creating new foci in other organs. Myxoma cells are also innocent in this sense. But this is where the deceptive nature of myxoma begins. Among medical professionals, we call it “functionally malignant”. This is due to the dangers posed by his behavioral pattern.
It can impair the function of the heart valves by preventing blood from flowing freely between the chambers. This causes your heart to work harder, tiring it out and eventually leading to the serious condition called heart failure. It is usually located in the left ear of the heart and attached to the wall by a thick stem. As it grows, it fills the left ear and can move and block the front of the mitral valve, mimicking mitral valve stenosis.
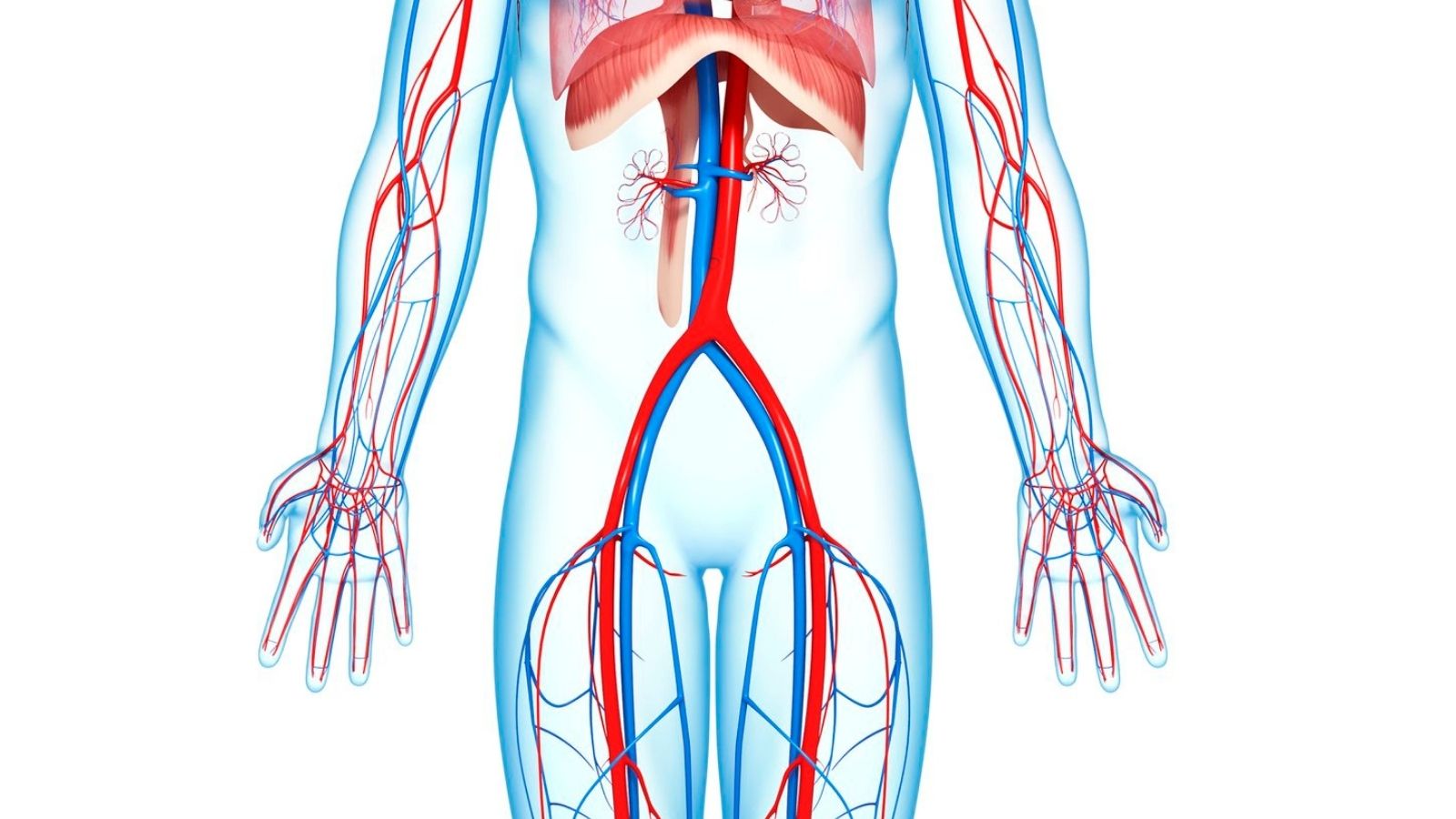
The main danger comes from the structure of the mixer. It is usually soft, friable and easily shattered. Small fragments of this gelatinous mass can break off with each beat of the heart. Caught in the bloodstream, these particles travel through the circulatory system like stray mines. Where this journey ends depends entirely on chance. If this is the money;
- If a blood vessel to the brain is blocked, a stroke occurs.
- If a blood vessel supplying the eye is blocked, sudden and permanent vision loss can occur.
- If it blocks the blood vessels supplying the kidney or spleen, infarction (tissue death) can occur in these organs.
- If the main artery to an arm or leg is blocked, the blood supply to that limb may be impaired, leading to gangrene.
Because of this potential for blood flow obstruction (obstruction) and clot formation (embolism), myxoma, although cellularly benign, is a condition that needs to be taken seriously and treated as soon as it is diagnosed.
How common is Cardiac Myxoma and who is at risk?
Cardiac myxoma is an extremely rare disease compared to the general population. The incidence rate in the general population is as low as one or two per hundred thousand. Although rare, when it comes to benign tumors that take root from the heart’s own tissue, myxoma is the most common type, accounting for more than half of these tumors.
It is commonly known as a middle-aged disease. It is most common in people between 30 and 60 years of age, with an average age of diagnosis around 50. Its occurrence in children is extremely rare. When a myxoma is detected in a child, it can often be a sign of an underlying genetic syndrome such as the “Carney Complex” and requires more detailed investigation.
An interesting feature of myxomania is its gender distribution. Although the cause is unknown, it is about two to three times more common in women than in men. This suggests that hormonal factors may play a role in tumor development, but this is not yet a proven theory.
What are the reasons behind myxoma formation?
The question of why myxomas arise is one of the most intriguing issues for patients. We can basically explain the development of these species by dividing them into two main categories:
Sporadic (Incidental) Myxomas: This group accounts for about -95% of all myxoma cases and is the most common type we encounter. the word “sporadic” means that the condition occurs by chance, without a specific family history or a known genetic predisposition. So in most of these patients, we cannot find a clear trigger factor to explain why the tumor developed.
Familial (Syndromic) Myxomas: A smaller proportion of cases, 5-10%, show a familial pattern. This is usually part of a genetic syndrome called the “Carney Complex”. This syndrome is a genetic disorder that can be passed from parent to child and causes problems in multiple systems in the body. People with Carney Complex may have tumors not only in the heart but also elsewhere in the body. Typical features of this syndrome include the following:
- Myxoma development in the skin and breast in addition to the heart
- Small, brown-black mottled spots on the lips, eyelids and genital area (lentigines)
- Tumors of the endocrine system causing hormonal disorders.
What are the main differences between Familial and Sporadic Myxoma?
Understanding whether a myxoma is sporadic or familial is vital to determine the follow-up plan after treatment. There are some clear differences between these two groups.
Characteristics of Sporadic Myxoma:
- It usually occurs between the ages of 40 and 60.
- It is more common in women.
- U of cases are located in the left ear of the heart.
- It usually takes the form of a single tumor.
- Once completely removed surgically, the risk of recurrence is very high.
Characteristics of Familial (Carney Complex) Myxoma:
- It is diagnosed at a much younger age, on average in the 20s.
- It occurs equally in men and women.
- It can be found in more unusual parts of the heart, such as the right atrium or ventricles.
- It can occur in more than one chamber at the same time or as new tumors at different times.
- Even after successful surgery, the risk of recurrence or the development of new tumors is significantly higher.
Therefore, when a myxoma is detected, especially in a young patient or in a location other than the left ear of the heart, the possibility of an underlying Carney Complex should always be investigated.
What are the symptoms of a myxoma?
The symptoms of myxomania can vary like a “chameleon”. Some patients may not experience any symptoms for years, while in others they may appear suddenly and with very severe symptoms. Symptoms usually depend on the size of the tumor, its location in the heart and how mobile it is. We can analyze the clinical picture under three main headings:
Symptoms of Heart Stricture:
These symptoms occur when the tumor, like a valve ball, blocks the opening of the heart valves or obstructs blood flow. It is particularly common in myxomas in the left auricle and may mimic signs of mitral valve stenosis. These are the symptoms that patients may experience:
- Shortness of breath that begins with exertion and over time is felt even at rest
- Increased feeling of suffocation, especially when lying on your back
- Shortness of breath and coughing attacks that wake you up at night
- Dizziness or darkening of the eyes caused by changing position (e.g., standing up suddenly)
- Fainting (syncope)
- Irregular heartbeats or palpitations
- Feeling of fullness or pressure in the mouth
Embolism (Clot Throwing) Symptoms:
This is the most dangerous and urgent consequence of myxoma. It occurs when a fragment breaks off from the tumor and blocks blood vessels. Symptoms vary depending on the location of the pinched vein.
Brain Embolism (Stroke):
- Sudden weakness or numbness on one side of the body
- Speech impediment or lisp
- Slippage in the mouth or face
- Blurred or double vision
- Severe dizziness and loss of balance
Other Organ Embolisms:
- Sudden and severe leg or arm pain, coldness, bruising
- Sudden darkening of the visual field or complete loss of vision
- Chest pain (can mimic a heart attack)
- Abdominal or flank pain (due to kidney or spleen damage)
Systematic (General Body) Symptoms:
About a third of patients may experience generalized symptoms similar to flu or rheumatic diseases due to the chemicals released by the tumor stimulating the immune system:
- Unexplained mild fever
- Weakness and constant fatigue
- Involuntary weight loss
- Joint and muscle pain
- Cold discoloration of the fingers (whitening, bruising)
- Skin rhombuses
These systematic symptoms usually disappear quickly after the tumor is surgically removed.
What methods are used to diagnose myxoma?
When a patient presents with a suspected myxoma, we work step by step to reach a diagnosis. The process starts with listening to the patient’s story and is refined with modern imaging technologies. The main methods used in the diagnostic process are as follows:
- Detailed Patient History and Physical Examination: Complaints such as shortness of breath, fainting, palpitations or a history of paralysis are our first clues. When we listen to the heart with a stethoscope, we can hear “murmurs”, which are abnormal sounds made by the blood as it passes around the tumor. Sometimes a very characteristic finding called “tumor plop”, the sound of the tumor hitting the heart wall, can also be detected.
- Echocardiography (ECHO): This is the cornerstone of myxoma diagnosis and is an ultrasound of the heart using sound waves. It is performed in two ways.
- Transthoracic ECHO (TTE): Standard ECHO through the chest wall is usually sufficient to show the presence, location and size of the tumor.
- Transesophageal Echo (TEE): When a more detailed view is needed, a probe with a small camera at the end is lowered into the esophagus. Because the heart is viewed from a much closer position, it provides an excellent view of details critical to surgery, such as where the tumor is attached, its structure and its relationship to the valves.
Cardiac Magnetic Resonance (MRI) and Computed Tomography (CT): These advanced imaging methods are used specifically to understand the tissue structure of the tumor and differentiate it from a blood clot or other type of tumor inside the heart. They provide a pre-operative “roadmap” for the surgeon, ensuring that the surgery is planned in the safest and most effective way.
Is there an option other than surgery to treat myxoma?

The answer to this question is clear: No. The only definitive treatment for cardiac myxoma is surgery. Because of the risks of sudden stroke, heart failure and death, a “wait and see” approach with medication is not an option. Once the diagnosis is made, the patient’s condition and the urgency of the tumor are assessed and surgery is planned as soon as possible.
The aim of the operation is to remove the tumor so that no fragments are left behind, along with the stem to which it is attached and a small amount of intact heart tissue. This minimizes the risk of the tumor recurring in the same place in the future.
Which surgical methods are preferred for myxoma surgery?
In the past, myxoma surgeries were performed with a large operation in which only the breast bone was completely cut, whereas today, it is completely removed with 4-5 cm minimally invasive surgery in the right armpit. With this method
- Minimal blood loss
- Shorter intensive care and hospital stay
- Reduced risk of infection
- Get back to everyday life and work much faster
- Excellent cosmetic results
Robotic Surgery:
This is the most advanced and technological form of minimally invasive surgery. The surgeon performs the surgery using robotic arms that he or she maneuvers through a console. Entering through only a few small holes (about 1 cm) in the chest wall, the robotic instruments offer precision and flexibility far beyond the mobility of the human hand. Under a three-dimensional and magnified image, the operation is completed with even the finest details visible. The advantages of robotic surgery take the benefits of minimally invasive surgery one step further. It ensures maximum safety and precision, especially in delicate maneuvers such as suturing and tissue repair.
What are the consequences of an untreated Myxoma?
An untreated myxoma is like a ticking time bomb. Over time, it will continue to grow and disrupt the structure of the heart, inevitably leading to serious complications. Knowing these risks is important to understand why treatment cannot be delayed. The most serious risks if left untreated are the following:
- Progressive and irreversible heart failure
- Permanent paralysis or disability as a result of a clot in the brain
- Tissue death in other organs (kidney, spleen, legs)
- Sudden and complete loss of vision
- A clot in the lung (pulmonary embolism)
- Flammulatory rhythm disturbances
- Sudden cardiac death
Cardiac myxoma is a rare but extremely serious condition. Fortunately, thanks to today’s modern diagnostic and therapeutic methods, this disease can be treated with a high success rate. Patient-friendly approaches such as minimally invasive and robotic surgery have made this process much more comfortable and safe. Remember that early diagnosis and timely and correct intervention can open the door to a healthy and long life.
After Myxoma Surgery
| The Progression of Renewal | Average 10-15 days. |
| The uniqueness of the whole | It is usually benign, located in the left atrium and may cause complications such as systemic embolism and valve obstruction. |
| Physical Activity | Light walking is recommended for the first 10-15 days; |
| Drug Use | Blood thinners, antibiotics or antiarrhythmic drugs may be routinely used; it depends on the individual case. |
| Monitoring and Control | Regular echocardiographic follow-up is recommended for the first year postoperatively, followed by annual check-ups. |
| Complications | Although rare, there is a possibility that myxoma may recur. In addition, rhythm disorders and valve problems may be observed after surgery. |
| Wound Care | not required after day 10 due to closed methods. |
| Nutrition | No special diet is required; a balanced and low-salt diet is recommended to protect heart health. |
| Psychological Support | Psychological support may be needed after a tumor diagnosis, especially in patients who have had an embolism. |
| Smoking and Alcohol | For the sake of heart health, smoking should be stopped and alcohol consumption should be limited. |
| Sexual Activity | It is usually possible after 4-6 weeks if physical improvement is achieved. |
| Tool Use | It can usually be started within 15 days after control of consciousness and reflexes has been achieved and physical recovery is complete. |
| Controls | Nuclear risk and cardiac function should be monitored by echocardiography once a month for the first 3 months and annually thereafter. |

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.