The aorta is the body’s main artery, responsible for carrying oxygen-rich blood from the heart to the entire body. An aortic tear occurs when the vessel wall weakens, leading to rupture or dissection. This condition is life-threatening and requires immediate medical attention.
Aortic aneurysm risk factors include uncontrolled hypertension, advanced age, smoking, and genetic connective tissue disorders. These factors weaken the aortic wall structure, increasing the chance of rupture. Preventive cardiology and regular imaging are vital for early detection.
Symptoms of an aortic tear usually begin suddenly with severe chest, back, or abdominal pain. The pain often radiates and can be accompanied by low blood pressure, shortness of breath, or loss of consciousness. Emergency diagnosis through imaging scans is essential for survival.
Treatment of an aortic rupture may include open surgery or endovascular repair, depending on the patient’s condition and tear location. Early intervention dramatically improves prognosis, while delayed treatment significantly increases mortality risk. Continuous follow-up is critical after repair.
| Medical Term | Aortic dissection |
| Definition | Serious, life-threatening condition that occurs when the inner layer of the aortic wall ruptures and blood enters between the layers of the wall |
| Classification | Stanford Type A: Rupture in the ascending aorta – Type B: In a ruptured descending aorta |
| Main Causes | Hypertension, Marfan syndrome, Ehlers-Danlos syndrome, trauma, bicuspid aortic valve, aortic aneurysm |
| Risk Factors | Age (especially over 60 years), male gender, smoking, family history, uncontrolled hypertension |
| Symptoms | Sudden onset, tearing, severe chest or back pain, syncope, shortness of breath, pulse difference, hypotension |
| Diagnostic Methods | Computed tomography angiography (CT angiography), transesophageal echocardiography, magnetic resonance angiography (MRI) |
| Treatment Methods | Type A: Emergency surgery – Type B: Medical treatment (blood pressure control) or endovascular intervention (TEVAR) |
| Complications | Aortic rupture, organ ischemia, stroke, cardiac tamponade, death |
| Urgent Intervention Necessity | Aortic dissection should be excluded in any patient with severe chest/back pain; urgent diagnosis and intervention are vital |
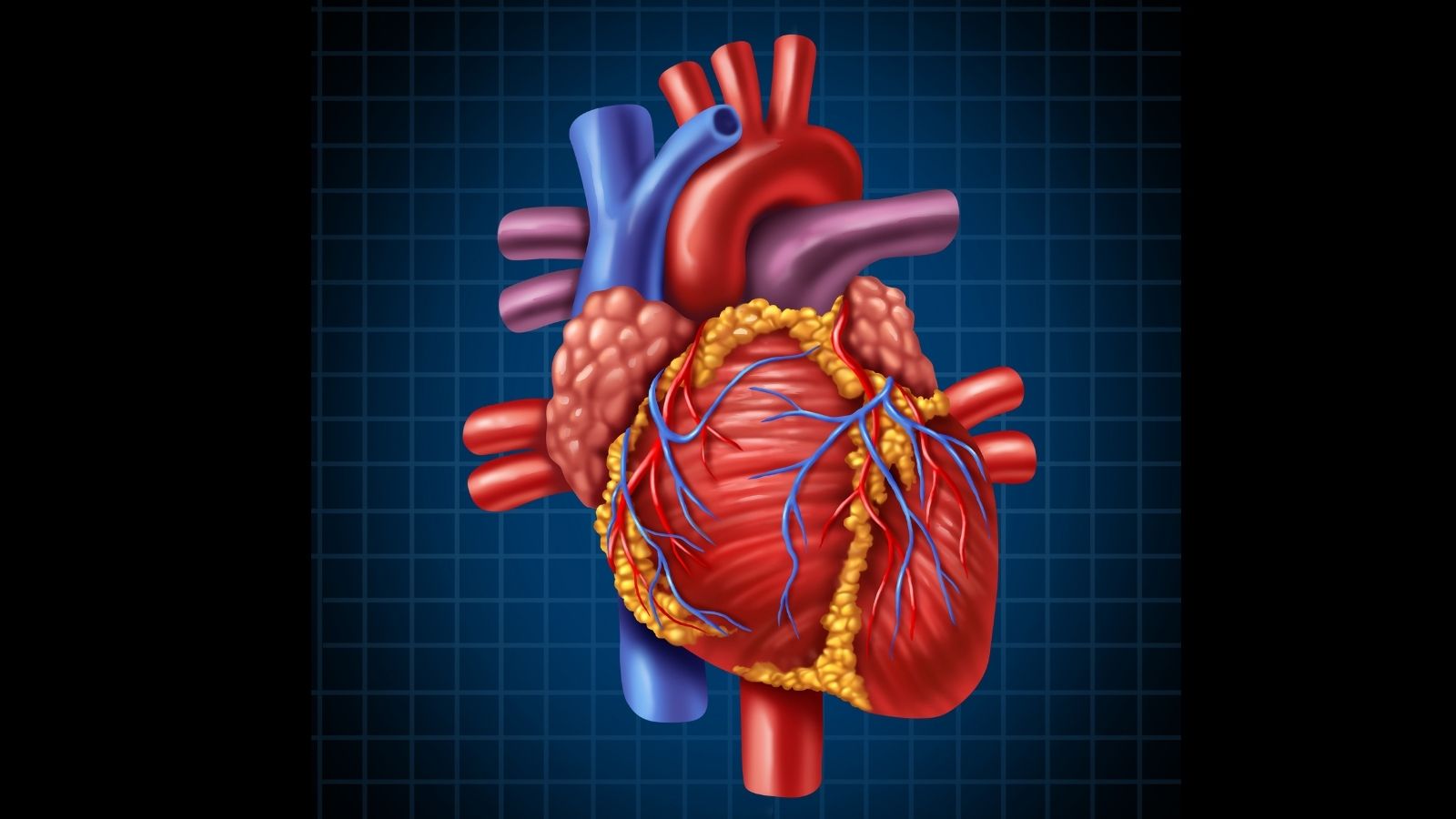
What is the Aorta and What is its Role in the Body?
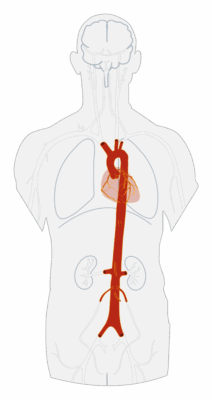
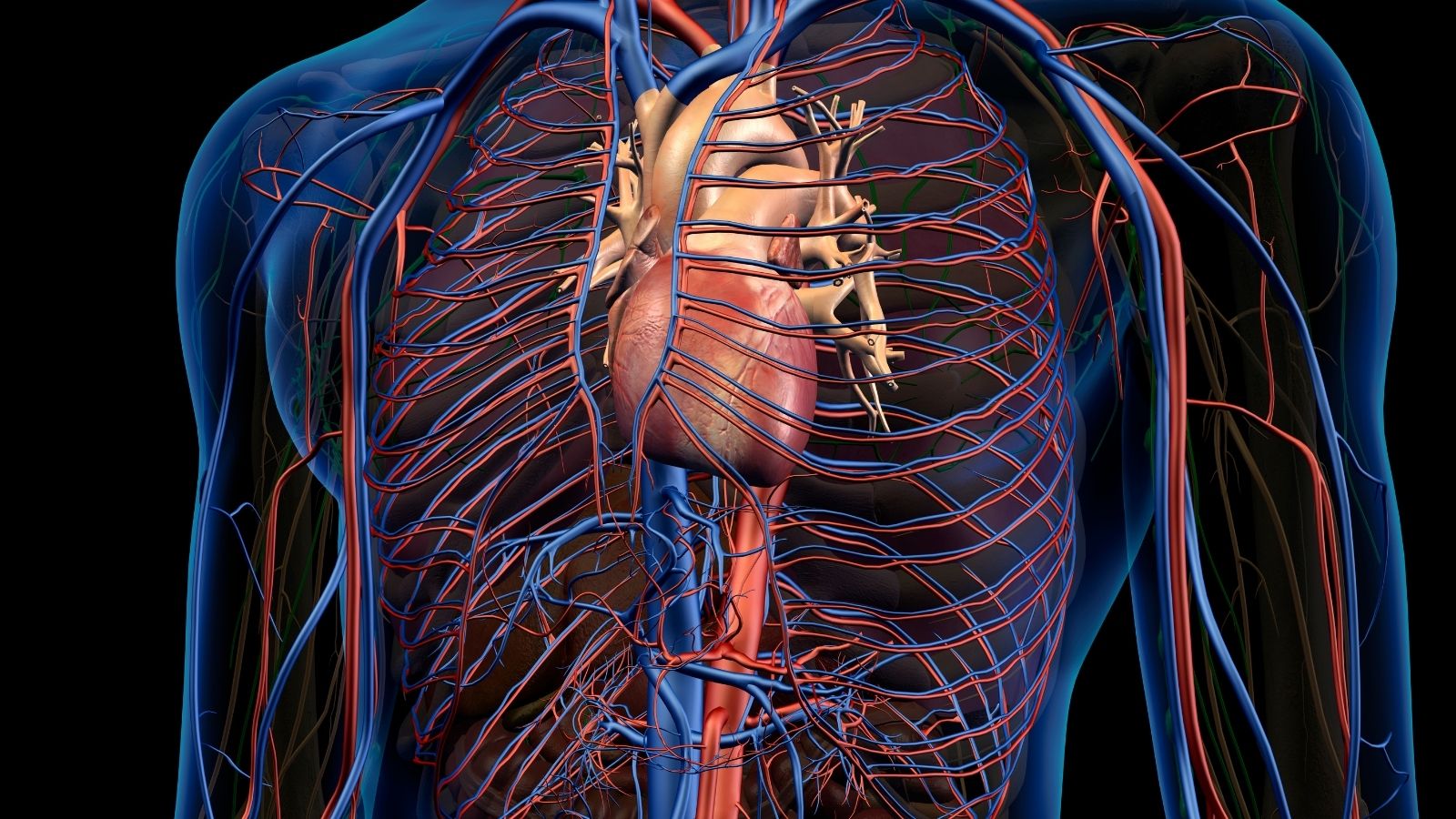
The aorta is a vital structure that originates in the lower left chamber (left ventricle) of the heart and is the largest artery in the body. Its main and most important job is to distribute the oxygen-filled blood that the heart receives with each pumping action to the most remote corners of the body. It is through this main distribution channel that the oxygen and nutrients your organs, muscles and tissues need to keep working are transported.
But the aorta’s role is not limited to this. It is not only a passive pipeline but also an intelligent manager at the center of the circulatory system. It helps stabilize blood pressure and delivers important chemical messengers, such as hormones, throughout the body. All the other arteries of the body are like smaller branches that branch off from the aorta. So even the slightest disruption in the health of the aorta can affect the entire system, jeopardizing blood flow and leading to life-threatening conditions within minutes. Therefore, it would not be wrong to consider aortic health as the basis of the health of the body as a whole.
Where is the Aortic Vessel Located and What is its Anatomy?
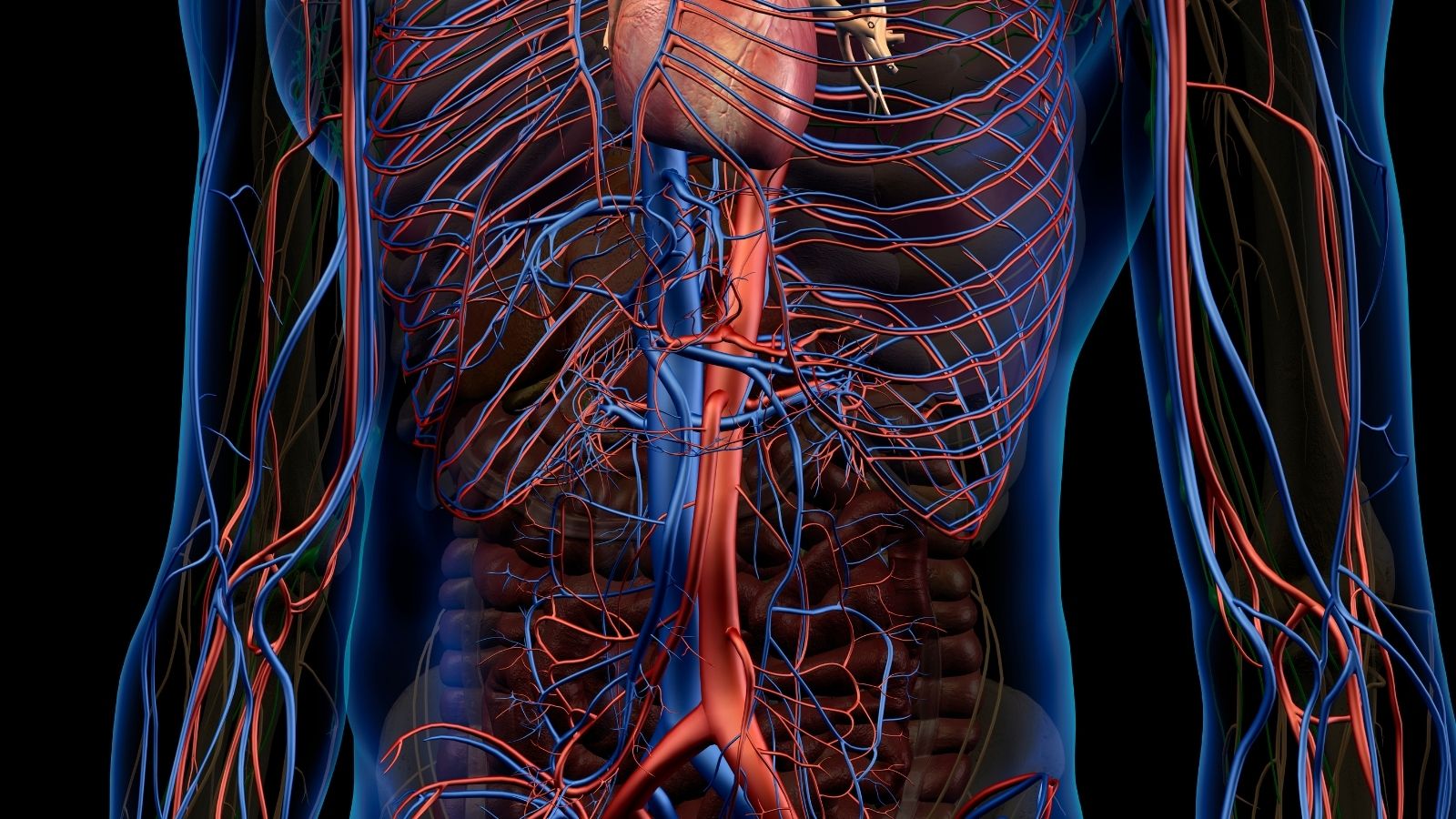
The aorta begins in the middle of the chest, curving like a cane after exiting the heart, and extends deep into the abdominal cavity. It is about 30 centimeters long and up to 2.5 centimeters in diameter at its widest point. The wall of this gigantic vessel is a perfect example of engineering, allowing it to both withstand high pressure and remain flexible.
The aortic wall is made up of three specialized layers:
- Tunica Intima (Inner Layer)
- Tunica Media (Middle Stratum)
- Tunica Adventitia (Outer Layer)
The inner layer is a slippery surface that allows blood to flow smoothly. Aortic rupture (dissection) is usually triggered by minor damage to this delicate layer. The middle layer is the thickest and strongest part of the wall. Its elastic fibers give the vessel its flexibility and allow the aorta to expand and contract slightly with each heartbeat. Diseases such as aneurysms and dissections are usually caused by the weakening and deterioration of this middle layer over time. The outermost layer is like a protective sheath that anchors the aorta to the surrounding tissues.
The main stops the aorta makes along its journey through the body are very important for us to determine the location and treatment of diseases:
- Aortic Root
- Ascending Aorta
- Aortic Arch
- Descending Aorta
The aortic root is the starting point where the artery leaves the heart and the coronary arteries that supply the heart leave. The ascending aorta is the part that runs upwards just behind the breastbone and is one of the most common sites of disease. The aortic arch is the curved section where the artery gives off critical branches to the brain and extremities. The descending aorta is the longest part of the aorta, running downward through the chest and abdominal cavity. Which of these departments the disease is in completely changes our treatment plan and its urgency.
What is Aortic Vessel Enlargement (Aneurysm)?
In its simplest definition, an aortic aneurysm is a permanent enlargement or ballooning that occurs at a weakened point in the vessel wall. The aortic wall, which is normally strong and flexible, can lose its integrity over time due to certain factors that disrupt its structure. This weak spot cannot withstand the constant pressure of the blood flowing through it and gradually begins to stretch outwards. When a blood vessel expands by more than P of its normal diameter, we medically call it an aneurysm.
This process can be likened to the thinning of the walls of an over-inflated balloon, increasing the risk of bursting. The larger the aneurysm, the thinner and more fragile the vessel wall and therefore the greater the risk of rupture. Aneurysms usually grow silently over many years without causing any symptoms. Regular check-ups are therefore vital for people in the risk group.
What is Aortic Vessel Rupture (Dissection)?
Aortic dissection is a sudden and dramatic event, very different from an aneurysm. In this case, a small tear occurs in the innermost layer of the vessel wall (intima). Blood flowing at high pressure seeps through this tear and enters between the layers of the vessel wall and begins to separate them. We can liken this to a multi-layered garden hose in which the inner layer is punctured and water accumulates between the layers, inflating the hose.
As the blood enters between the layers of the wall, it creates a second channel called the “false lumen”. This false channel widens as it fills with blood, squeezing and narrowing the “true lumen” through which blood should normally flow. This compression can block the mouths of the vessels that branch off from the aorta and lead to vital organs such as the brain, heart, kidneys or legs. As a result, depending on which vessel is blocked, the patient may present with a sudden stroke, heart attack or organ failure. Aortic dissection is therefore seen as a vascular catastrophe with sudden onset and devastating consequences.
What is a burst aortic vessel (rupture)?
Aortic rupture is the last and most deadly stage of aortic disease. In this case, the weakened and perhaps delaminated aortic wall can no longer withstand the blood pressure inside and ruptures completely. This is a full-fold bursting of the vessel. The blood drains uncontrollably into the chest or abdominal cavity. This leads to massive internal bleeding, often resulting in shock and death within seconds or minutes.
So, can a burst aortic artery kill? The answer to this question is, unfortunately, a sad yes. More than half of patients with aortic rupture die before they even reach the hospital. Even in those who reach the hospital, the mortality rate is very high. That is why when an aneurysm or dissection is diagnosed, all our efforts, treatment and follow-up are focused on preventing this ultimate and catastrophic event from happening.
What Causes Aortic Rupture and Enlargement?
So why do the walls of this sturdy highway weaken? There is no single answer to the question of why the aorta ruptures or dilates. It is usually triggered by a combination of multiple underlying factors. The main reasons behind this weakening are the following:
- Atherosclerosis (Arteriosclerosis)
- Uncontrolled High Blood Pressure (Hypertension)
- Genetic Connective Tissue Diseases
- Bicuspid Aortic Valve
- Traumatic Injuries
- Infection and Inflammation
Arteriosclerosis is the most common cause of aneurysms, especially in the abdomen. Over the years, fat and lime plaques build up on the vessel wall, causing it to lose its elasticity. High blood pressure acts like a constant hammer blow on the aortic wall. This incessant mechanical stress frays and weakens the fibers of the wall. Some genetic diseases, such as Marfan syndrome, leave a person with a congenitally weak aortic wall, which increases the risk of rupture even at a very young age.
What are the Risk Factors for Aortic Vessel Diseases?
In addition to direct causes, certain habits and characteristics increase your chances of developing aortic diseases. Knowing these risk factors is important to take precautions and understand who needs to be more careful.
Here are some important risk factors that depend on your lifestyle and that you can control:
- Smoking and Tobacco Use
- Uncontrolled High Blood Pressure
- High Cholesterol
Smoking is the strongest and most dangerous known risk factor for aortic diseases. It directly weakens the vessel wall, multiplying the risk of aneurysm formation and bursting many times over.
Some risk factors are beyond your control and these people need to be more aware:
- Advanced Age (usually over 60 years)
- Male Gender
- Family History (aneurysm in first-degree relatives)
- Genetic Syndromes (Marfan, Loeys-Dietz etc.)
What are the Symptoms of Aortic Vessel Enlargement (Aneurysm)?
The most dangerous aspect of aortic aneurysms is that they usually grow silently for years without any symptoms. This is why they are called “silent killers”. They are often discovered by chance during an ultrasound or CT scan when a doctor visits with another complaint.
However, when the aneurysm grows and starts to put pressure on the surrounding tissues, it may give some vague signals depending on its location. Symptoms of abdominal (abdominal) aortic aneurysms are as follows:
- Deep, gnawing pain in the abdomen or back
- A lump or pulsating sensation around the navel that beats with your heart (throbbing)
In thoracic aneurysms, the following symptoms may occur depending on the compression of neighboring organs:
- Chest pain
- Pain in the back, especially between the shoulder blades
- Unexplained shortness of breath
- Hoarseness
- Difficulty swallowing
These symptoms can often be mistaken for other diseases. Therefore, screening people at risk (especially men over the age of 65 and smokers) is the most effective way to detect this silent danger early.
What are the Symptoms of Aortic Tear (Dissection) and Rupture (Rupture)?
In contrast to the silence of an aneurysm, dissection and rupture often present with dramatic, sudden and frightening symptoms. Anyone experiencing these symptoms should contact the nearest emergency room without losing a second.
Symptoms of aortic dissection start suddenly and are very severe. The most common alarming signs are the following:
- Sudden, tearing or stabbing chest or back pain
- Fainting, feeling like fainting or sudden loss of consciousness
- Severe shortness of breath
- Cold sweats, nausea and vomiting
- Weak or absent pulse in one arm or leg compared to the other
- Stroke-like symptoms (facial shift, slurred speech, weakness in the arm or leg)
The location of the pain also gives us an important clue as to where the tear is located. Pain in the front of the chest usually points to the ascending aorta, while back pain points to the descending aorta. Aortic rupture is the most severe form of these symptoms. The patient develops a sudden drop in blood pressure, shock and rapid loss of consciousness.
How Are Aortic Vessel Diseases Diagnosed?
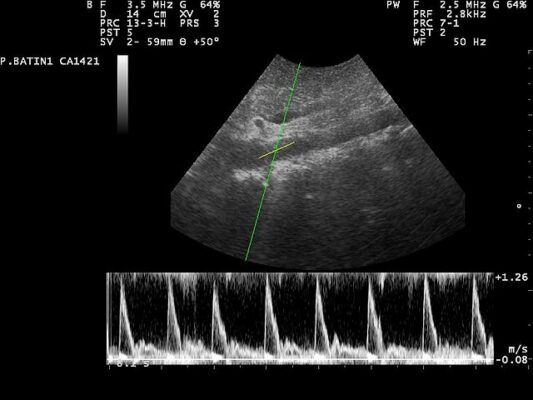
When we suspect aortic diseases, the patient’s story and examination findings are very important. However, the modern imaging methods we use to make a definitive diagnosis and draw our road map are the following:
- Ultrasonography (USG) and Echocardiography (ECHO)
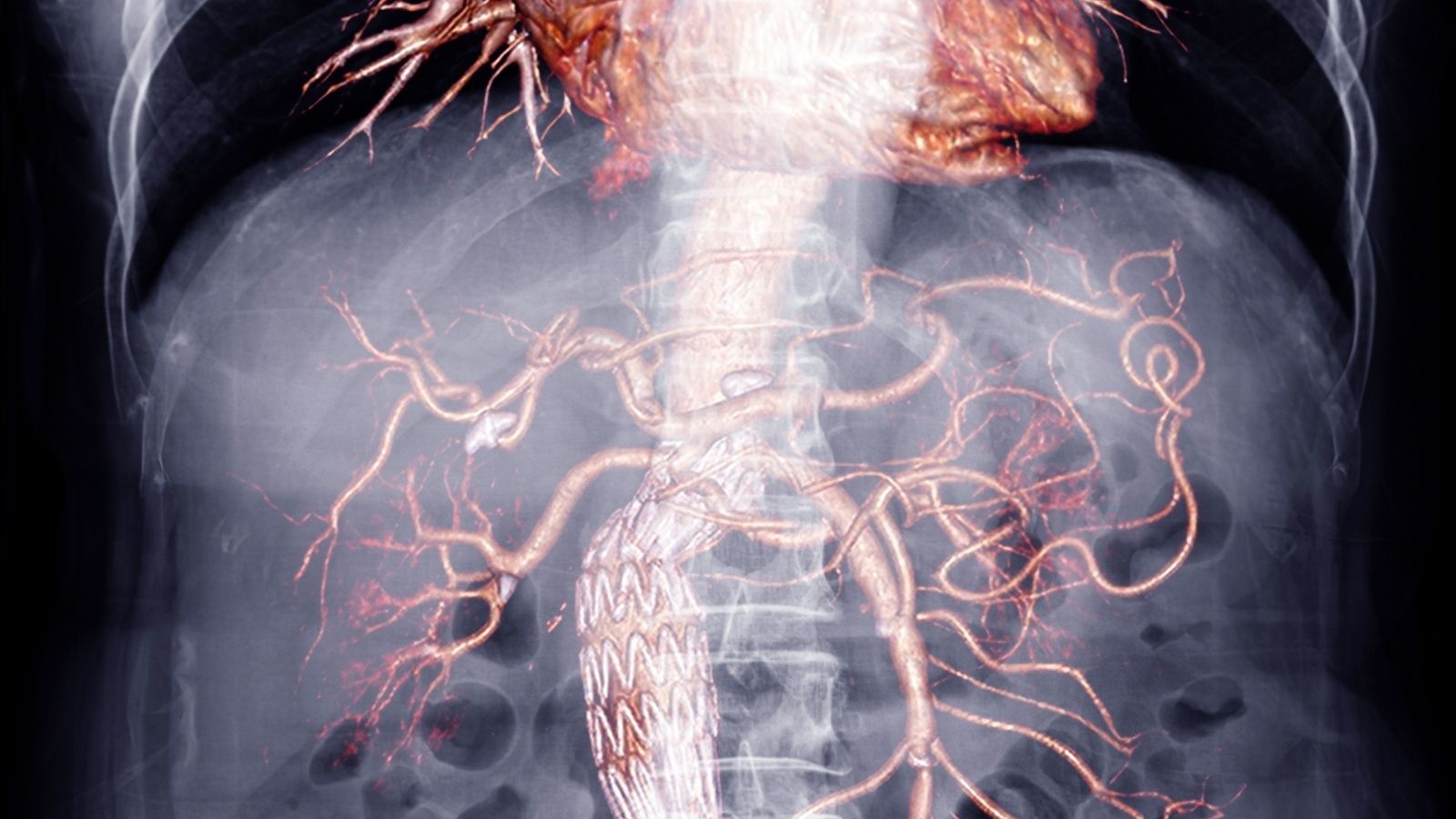
- Computed Tomography Angiography (CTA)
- Magnetic Resonance Angiography (MRA)
Ultrasound is a harmless and practical method, especially for screening and monitoring abdominal aneurysms. Echocardiography (ECHO), i.e. ultrasound of the heart, gives us quick information to evaluate the first part of the aorta that exits the heart. ECHO (TEE), especially through the esophagus, shows the thoracic aorta very clearly.
However, in emergencies and for surgical planning, the gold standard method is Computed Tomography Angiography (CTA). This test, in which a special drug (contrast agent) is administered intravenously, maps the entire aorta in three dimensions. In seconds, it gives us the exact location of the tear, the size of the aneurysm, the condition of the branches to the organs and all the critical information needed for treatment. Magnetic Resonance Imaging (MRA) is a valuable alternative that we prefer especially in young patients or in cases where regular follow-up is required because it does not involve radiation.
What are the Differences between Open and Closed Methods in Aortic Valve Surgery?
There are basically two main approaches to the surgical treatment of aortic disease: open surgery and endovascular (closed) repair. Which method is chosen depends on the patient’s age, general health and the location and shape of the aneurysm or tear. It is a tailor-made decision.
Open surgical repair is the traditional and gold standard method that has been used for many years with proven results. In this operation, we make an incision in the chest or abdominal wall, depending on where the aneurysm is located, and access the vessel directly. We completely remove the diseased, weakened aortic section and replace it with an artificial vessel (graft) made of a very durable synthetic material such as Dakron. This method offers the most durable solution in the long term, especially in young patients in good general health. However, since it is a major surgery, the recovery period is longer.
Endovascular repair (EVAR/TEVAR) is a more modern and less invasive technique. Instead of making a large incision, we usually enter through a small hole in the groin artery. Using an angioplasty-like method, catheters are inserted through the vein to reach the site of the aneurysm. Here we insert a “stent-graft”, which is a fabric tube supported by a metal framework (stent). This stent-graft covers the inside of the aneurysm, creating a new, solid tunnel for blood flow. This prevents the blood from pressing against the weakened aneurysm wall. This is a great alternative, especially for elderly patients or patients with comorbidities who are at high risk for open surgery. Recovery is much faster and more comfortable, but requires lifelong follow-up with regular monitoring.
What is the Recovery Process After Aortic Vessel Rupture Surgery?
Recovery after aortic surgery differs significantly depending on the surgical method used. However, in both cases, it is important to know that this process is a marathon that requires patience and care. Immediately after surgery, our patients spend a few days in the intensive care unit where all vital functions are monitored moment by moment. This is the most critical first step in recovery.
Once the patient is stabilized, he/she is taken to the surgical ward. Our aim here is to gradually get the patient up on his/her feet, walking and encouraging him/her to eat normally. While the average hospital stay after open surgery is one week, this period is usually 1-3 days after the closed method.
The recovery period at home is when patience is required. While full recovery after open surgery can take 2-3 months, this period is approximately 4-6 weeks after endovascular repair. Fatigue, loss of appetite and mild pain at the incision site are normal during this period. It is especially important for patients who have undergone open surgery to avoid lifting, pushing or pulling anything heavier than 5 kilograms for about 4-6 weeks to allow the sternum or abdominal bone to fully fuse. Short and regular daily walks are the best medicine to speed up recovery by increasing blood circulation and strengthening muscles.
Is it Possible to Prevent Aortic Vessel Diseases or Prevent Recurrence?
Absolutely yes. You cannot change your genetic inheritance, but you can have tremendous control over your aortic health through your lifestyle. For someone who has been diagnosed with aortic disease or has had surgery, these steps are part of the treatment and prolong the life of the repair. For a person at risk who has not yet experienced a problem, these steps are the most effective way to prevent a potential disaster.
Here are the most important steps you can take to protect your aortic health and prevent possible worst-case scenarios:
- Quit smoking absolutely and immediately
- Keeping blood pressure at an ideal level (usually around 12/8)
- A low-salt, Mediterranean-type diet
- Maintaining ideal weight
- Regular and moderate exercise every day (walking, swimming, etc.)
- Avoiding activities that require sudden exertion such as heavy lifting
- Having regular screening tests if you are in a risk group
- Do not interrupt the medications prescribed by your doctor and do not neglect follow-ups
Remember, aortic health is a team work. The most important member of this team is you and the other is your physician. In this long-term partnership, taking an active role in your own health is the key to a long and healthy life.
Frequently Asked Questions
What is a ruptured aorta?
Aortic rupture is a life-threatening condition that occurs when the inner layer of the aorta, the largest artery in the body, ruptures and blood travels through the vessel wall.
Is aortic dissection the same as aortic rupture?
Yes, this condition, medically called “aortic dissection”, is commonly referred to as “aortic rupture”.
What causes a ruptured aorta?
It can develop after hypertension, arteriosclerosis, genetic connective tissue diseases (such as Marfan syndrome), trauma or heart surgery.
What are the symptoms of a ruptured aorta?
Sudden onset of very severe chest or back pain that feels like tearing, shortness of breath, fainting and low blood pressure are common.
Is a ruptured aorta an emergency?
Yes, it is a very serious and potentially fatal emergency. Intervention in the first hours is life-saving.
Who is more prone to aortic rupture?
it is more common in men over 50, those with long-term hypertension, and those with a history of vascular disease.
How is a ruptured aorta diagnosed?
Definitive diagnosis is made with imaging methods such as CT angiography (tomography), ECHO and MRI.
Is a ruptured aorta similar to a heart attack?
Yes, the symptoms may be similar but the treatment approaches are very different. Therefore, rapid diagnosis is very important.
Can aortic rupture be treated without surgery?
For Type B dissections (when only the aorta outside the chest is affected), medication may be sufficient. However, Type A dissections (the first part to exit the heart) usually require surgery.
What is the risk of death in aortic rupture?
It is very high. Without intervention in the first 24 hours, the mortality rate increases by 1% per hour.
How is life affected after a ruptured aorta?
Life can be sustained with early and correct intervention. However, regular follow-up and blood pressure control is essential.
Will someone who has had an aortic rupture experience the same risk again?
Yes, if the vessel wall is weak, new ruptures or dilatations can occur. Continuous monitoring is therefore important.
How to prevent aortic rupture?
The risk can be reduced by keeping blood pressure under control, healthy lifestyle, smoking cessation and regular cardiologic follow-up.
Which doctors are consulted for a ruptured aorta?
It is evaluated and treated by specialists in cardiology, cardiovascular surgery and emergency medicine.
Is there a link between aortic tear and EVAR/TEVAR?
Yes. In appropriate cases, the ruptured aortic area can be closed repaired with stenting methods called EVAR or TEVAR.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.