The circulatory system is responsible for transporting oxygen, nutrients, and hormones while removing metabolic waste products. It consists of the heart, blood, and vascular network.
Cardiovascular diseases such as coronary artery disease, hypertension, and heart failure are major health problems worldwide. They often result from atherosclerosis, lifestyle factors, or genetic predisposition.
Peripheral vascular diseases affect arteries and veins outside the heart, leading to symptoms like leg pain, swelling, or ulcers. Early detection and treatment improve quality of life and reduce complications.
Prevention of circulatory system diseases relies on healthy lifestyle choices, regular exercise, smoking cessation, and management of risk factors such as diabetes and high cholesterol.
| Medical Name | Circulatory System (Cardiovascular System) |
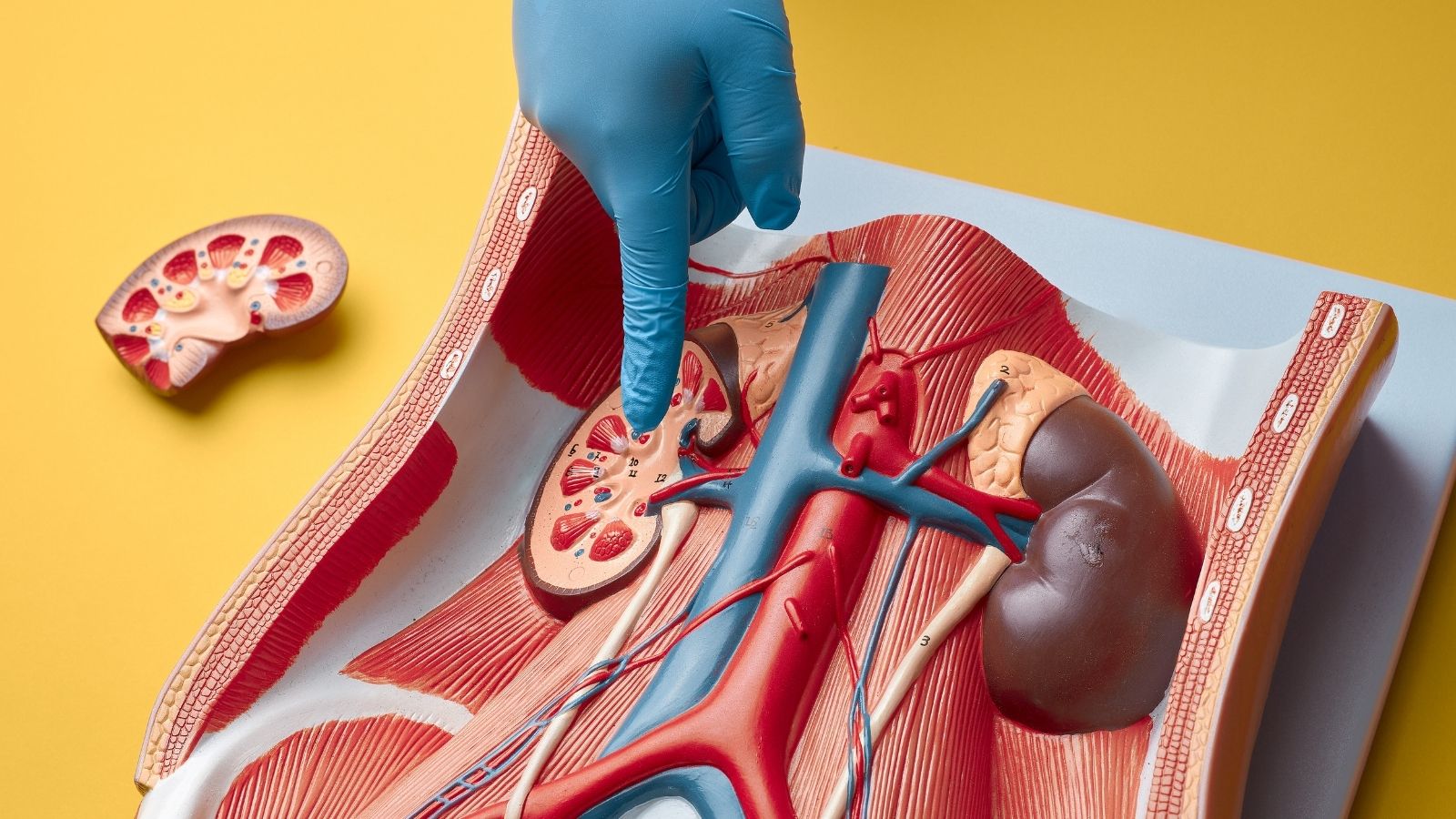
| Main Organs | – Heart- Arteries (arteries) – Veins (veins) – Capillaries |
| Duties | – Transportation of oxygen and nutrients to tissues – Removal of carbon dioxide and waste materials – Hormone and heat distribution |
| Common Diseases | – Hypertension- Coronary artery disease- Heart failure- Varicose veins- Peripheral artery disease |
| Risk Factors | – Obesity- High blood pressure- Diabetes- Smoking and alcohol use- High cholesterol- Physical inactivity |
| Complications | – Heart attack – Stroke – Impaired circulation in organs – Ulcers and wounds on legs |
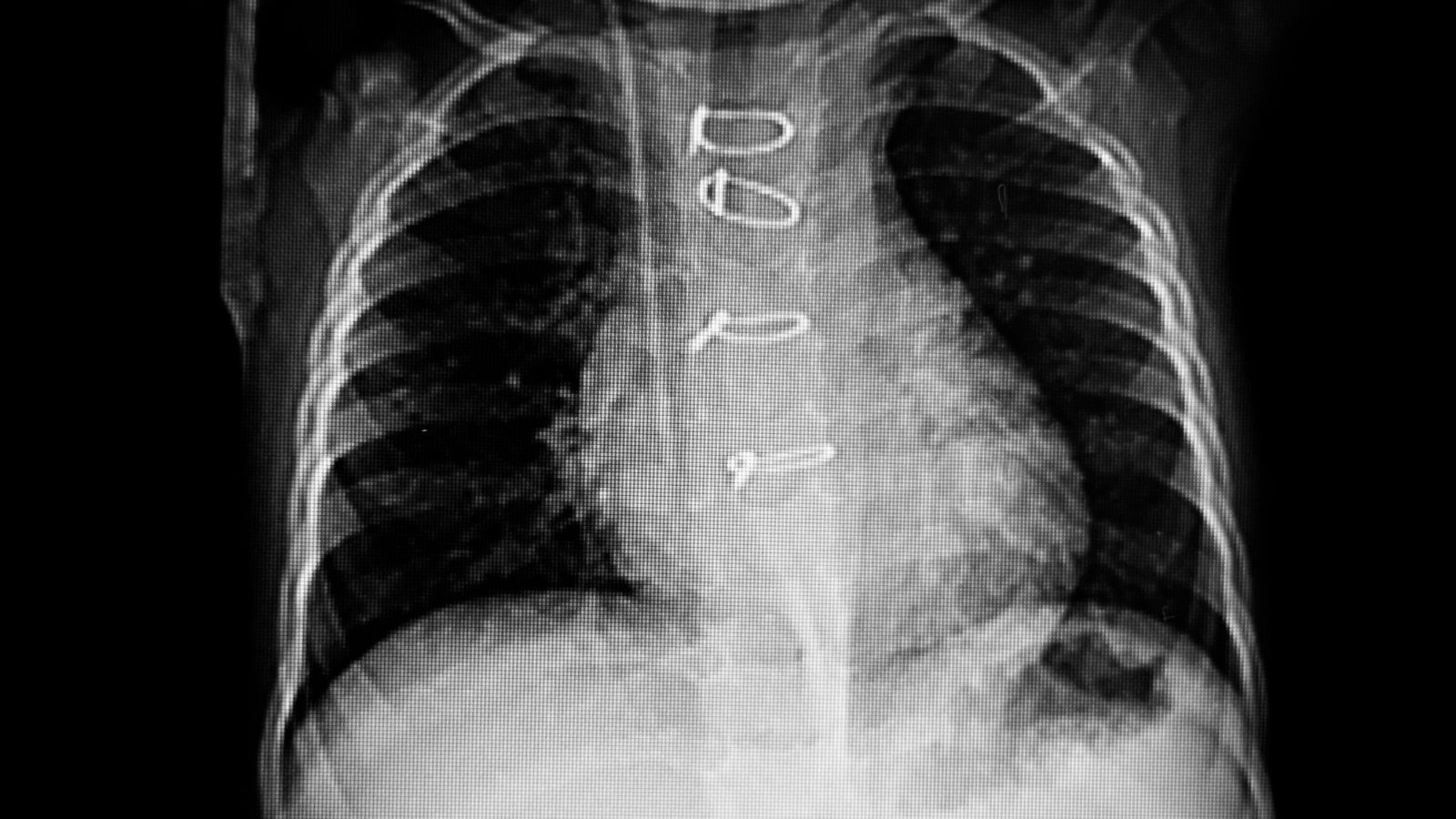
| Diagnostic Methods | – Physical examination- ECG- Echocardiography- Angiography- Blood tests- Doppler ultrasonography |
| Treatment Methods | – Lifestyle changes (diet, exercise)- Medication (blood pressure, cholesterol, blood thinners)- Surgical or interventional procedures (stent, bypass, etc.) |
| Prevention Methods | – Healthy diet- Regular exercise- Quitting smoking and alcohol- Regular control of blood pressure, sugar and cholesterol |
How Does the Circulatory System, the Engine of Our Body, Work?
We can liken the circulatory system to an orchestra. The conductor of this orchestra is the heart and the musicians are the arteries, veins and capillaries. They all work in perfect harmony with each other to maintain the melody of our life.
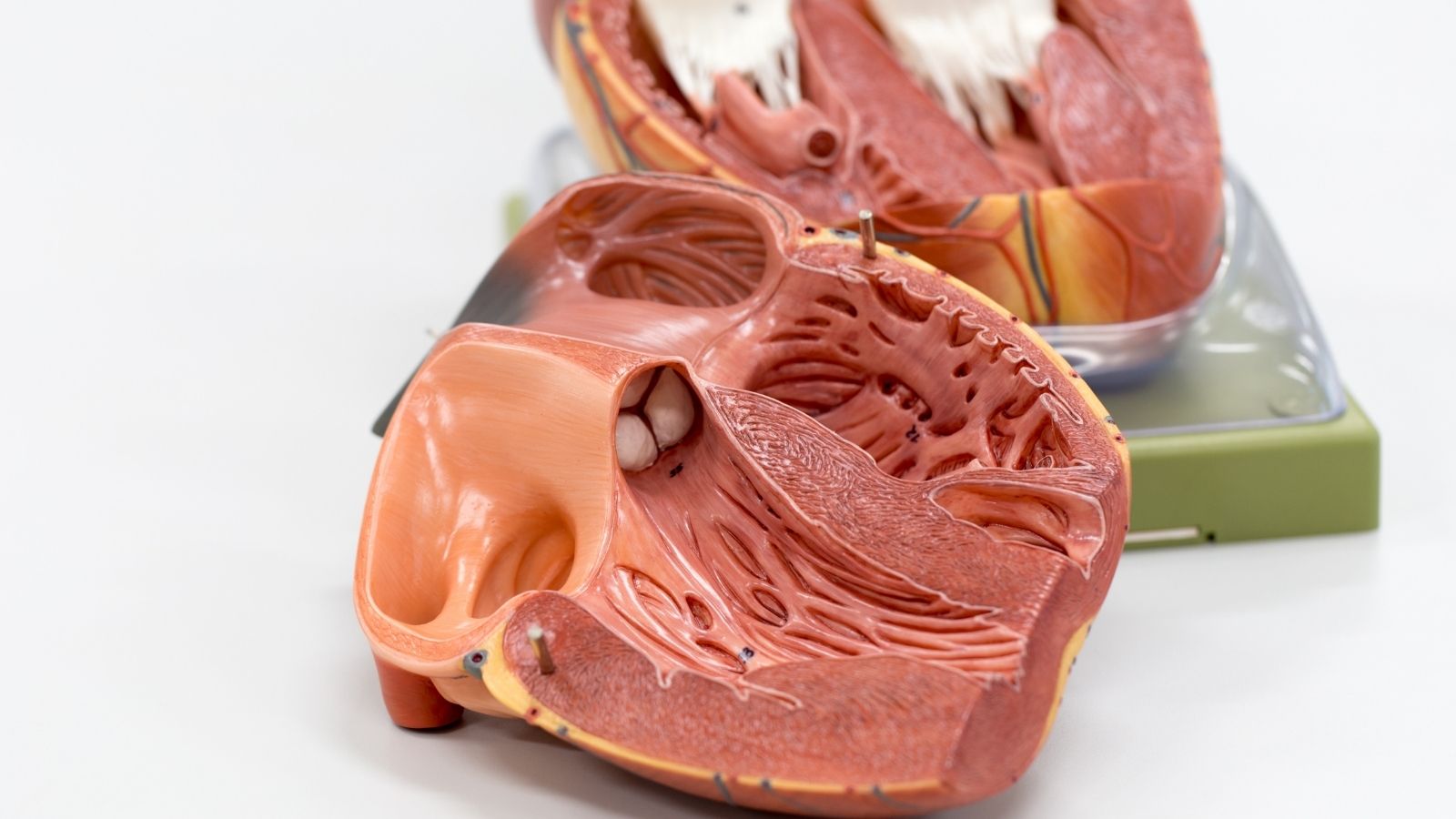
The heart, the muscular organ at the center of our rib cage, the size of an average fist, is the tireless engine of this system. Its main task is to pump blood non-stop. It accomplishes this task thanks to its four-chambered structure. Blood that has been used in the body and has lost its oxygen comes into the right atrium of the heart through the main veins. From there it passes to the right ventricle and is sent to the lungs to be cleaned. Filled with fresh oxygen in the lungs, the blood returns to the left atrium of the heart. The last stop is the left ventricle, the strongest and most muscular part of the heart. The left ventricle contracts with great force to pump this clean blood into the aorta, the body’s main artery, from where it begins its journey to all organs and tissues.
During this journey, there are four valves that keep the blood flowing forward, in the right direction. These valves are like delicate gates between the chambers and at the exit of the great vessels, preventing blood from escaping backwards. Their regular opening and closing is critical for the efficient operation of the system.
The vessels are the pathways of this system. We can divide them into three main groups. Arteries are thick-walled, strong pathways that take clean blood from the heart and distribute it throughout the body. Veins are thinner-walled return pathways that collect used blood and bring it back to the heart. Capillaries are the invisibly thin alleyways that connect these two networks of pathways. It is in these capillaries that the real miracle takes place, where oxygen and nutrients are released into the tissues and waste is taken up into the blood. All these circulatory systems in our body are divided into two main lines, the small and the large circulation, and work in an uninterrupted cycle throughout life.
What are the Symptoms of General Circulatory System Diseases?
Our body sends us signals when something is wrong. Problems with the circulatory system often manifest themselves with some common symptoms. Recognizing these symptoms early is vital for accurate diagnosis and treatment. Some common symptoms include:
- Shortness of breath (especially with exertion or lying down)
- Pressure, tightness or pain in the chest
- Swelling in the legs or ankles (edema)
- Cramp-like pain in the legs or buttocks when walking
- Dizziness or fainting
- Palpitations or a feeling that the heart is beating irregularly
- Fatigue and weakness more quickly than usual
- Persistent coldness or bruising of the hands and feet
- Wounds that do not heal (especially on the legs)
If you experience one or more of these symptoms, it does not necessarily mean that there is a serious problem. However, the best approach is not to ignore these signals and to consult a physician. Sometimes a very mild symptom can be the first harbinger of a progressive disease. Early diagnosis is the most important factor directly affecting the success of treatment.
What is Coronary Artery Disease, the Most Common Circulatory System Disease?
While the heart pumps blood throughout the body, it also needs nourishment. This is done by special arteries called “coronary arteries”, which lie like a crown on the surface of the heart. Coronary artery disease is the narrowing or blockage of these arteries over time. It is one of the most common and most serious circulatory system diseases worldwide.
The underlying process of this disease is “atherosclerosis”, or arteriosclerosis. We can liken this to the accumulation of lime in the clean water pipes in our homes over time. Over the years, especially under the influence of factors such as high cholesterol, smoking, high blood pressure and diabetes, fatty and calcareous deposits called “plaques” form on the inner wall of the arteries. As these plaques grow, they narrow the inside of the artery and block blood flow to the heart.
The heart muscle needs more oxygen, especially when we exert ourselves (climbing stairs, walking fast, etc.). When the narrowed blood vessel is unable to meet this demand, the typical pain known as “angina pectoris” occurs, which is characterized by a feeling of pressure or tightness in the chest. If a plaque suddenly ruptures and a clot quickly forms on it and completely blocks the blood vessel, this leads to a heart attack (myocardial infarction). A heart attack means that the muscles in that area of the heart are permanently damaged and requires emergency intervention.
What are the Risk Factors for Circulatory System and Blood Diseases?
There are some risk factors that affect the health of our blood vessels and therefore the future of our circulatory system. We can divide these into two main groups: those we can change and those we cannot. The important thing is to minimize our risk by controlling the factors we can change.
The risk factors we can change (controllable) are:
- Smoking and use of tobacco products
- High blood pressure (Hypertension)
- High blood cholesterol and triglyceride levels
- Diabetes (Diabetes)
- Overweight and obesity
- A sedentary lifestyle
- Unhealthy eating habits
- Intense and unmanageable stress
Risk factors that we cannot change (cannot be controlled) are as follows:
- Advanced age
- Male gender (risk increases in women after menopause)
- Family history of heart disease at an early age (genetic predisposition)
When several of these risk factors come together, they accelerate the process of atherosclerosis by amplifying the negative effects of each other. For example, a diabetic smoker’s risk of having a heart attack increases exponentially compared to someone with only one risk factor. Therefore, lifestyle changes and regular medical check-ups are of great importance.
What Does Circulatory System Medicine Offer in the Treatment of Coronary Artery Disease?
If the stenosis in the coronary arteries is too severe to be overcome with medication or stents, the most effective and permanent solution is usually surgery. This is where “coronary artery bypass surgery” comes in. The rationale for the operation is simple: to create a new pathway, a bridge (bypass), to bring blood across the blocked artery. This revitalizes areas of the heart muscle that have been deprived of blood.
For this bridging procedure, veins taken from the patient’s own body are usually used. Some of the graft (vein) types used are as follows:
- Chest wall artery (the left side is most commonly used and is known as LIMA)
- Artery from the arm (radial artery)
- Vein taken from the leg (saphenous vein)
The most valuable of these grafts is the artery taken from the chest wall. Because the structure of this vessel has a natural resistance to arteriosclerosis and has a very high rate of remaining open for years. Therefore, the use of this graft, especially in the most important vessel of the heart, directly affects the long-term success of the surgery.
Bypass surgery is traditionally performed by stopping the heart and connecting the patient’s blood to a heart-lung machine. This method allows the surgeon to make extremely precise sutures, even in very thin vessels, in an immobilized and bloodless area. However, in some high-risk patients, the “bypass on a working heart” technique may be preferred to avoid the potential side effects of the heart-lung machine. In this technique, only a small area of the heart to be sutured is stabilized with the help of special instruments and the operation is performed while the heart continues to beat in its normal rhythm. Which technique to choose is a decision made jointly by the “Heart Team” based on the general condition of the patient, the structure of the vessels and the experience of the surgeon.
What Are Valvular Heart Diseases, a Type of Circulatory System Disorders?
The four valves inside our heart are like one-way doors that regulate blood flow. These valves can develop problems over time or due to congenital causes. These problems usually manifest themselves in two ways: stenosis (stenosis) or regurgitation (leakage). In stenosis, the valve cannot open fully and it is difficult for blood to pass forward. In regurgitation, the valve cannot close completely and blood leaks backwards. Both conditions cause the heart to work harder than normal, become fatigued and eventually enlarge, leading to heart failure. The aortic and mitral valves, in particular, are the most commonly affected by such diseases.
How is Aortic Valve Disease Treated?
The aortic valve is the main outlet through which fresh blood is pumped from the heart throughout the body. Stenosis or insufficiency of this valve is of vital importance. The aim of treatment is to lighten the burden on the heart and improve the patient’s quality of life.
The traditional and gold standard treatment is “surgical aortic valve replacement”, i.e. open heart surgery to remove the diseased valve and replace it with a prosthetic valve. There are two types of valve options in this surgery and the choice is based on the patient’s age, lifestyle and expectations.
The characteristics of mechanical covers are as follows:
- The material is titanium and carbon.
- Durability is for life.
- Lifelong use of blood thinners is mandatory to prevent clotting.
- It is generally preferred in young patients under the age of 65 who do not mind using blood thinners.
The features of biological valves are as follows:
- Produced from bovine or porcine heart membrane.
- Its durability is limited to 10-20 years.
- Generally does not require blood thinners.
- Suitable for elderly patients or patients who cannot take blood thinners.
In recent years, a new method called “TAVR” has been developed especially for patients at high risk of surgery. TAVR is a procedure in which a catheter is inserted through the groin to deliver a new biological valve to the heart and insert it into the diseased valve. This method avoids the need for open heart surgery. Today, the use of TAVR has expanded to intermediate and even low-risk patients thanks to successful results. The “Heart Team”, consisting of cardiac surgeons, cardiologists and other specialists, decides together which method is most appropriate for a patient (surgery or TAVR?).
What is the Circulatory System Approach to Mitral Valve Disease Management?
The mitral valve, on the left side of the heart, controls the passage of clean blood from the lungs to the final chamber where it is pumped into the body. It is a common problem for this valve to leak blood, especially backwards (mitral regurgitation). The modern approach to the treatment of mitral valve disease is to “repair” the valve rather than replace it, if possible.
Valve repair offers many advantages because it preserves the patient’s own tissue. These include a lower risk of surgery, better preservation of the heart’s natural structure and function, and no need to use blood thinners. Valve repair is a tailoring process. The surgeon repairs the damaged parts of the valve, supports it with artificial strands (chordae) if necessary and sews a ring (annuloplasty ring) around the valve to make the repair permanent.
Some common techniques for mitral valve repair are as follows:
- Reshaping of sagging or too mobile parts of the valve
- Replacement of broken or elongated cover strands with artificial ones
- Supporting the enlarged valve ring by narrowing it with a ring
- Opening of adhered valves
These delicate repair procedures can now be performed not only by opening the rib cage completely, but also through a small incision on the right side (minimally invasive surgery) or “robotic surgery”. Robotic surgery is a three-dimensional and magnified image of the operation, which is performed through several small punctures, using robotic arms directed by the surgeon from a console. This method offers the surgeon a precision and mobility beyond the reach of the human hand, while for the patient it means less pain, faster recovery and better cosmetic results.
What are the Circulatory System Diseases of the Aorta, the Main Artery of the Body?
The aorta is the largest artery in our body and is the main line that distributes blood from the heart to all organs. Problems in this giant vessel threaten the entire circulatory system. The two most common main aortic diseases are aneurysm and dissection.
An aortic aneurysm is when the wall of the aorta weakens and expands like a balloon. This ballooning can occur in the abdomen (abdominal aortic aneurysm) or in the chest (thoracic aortic aneurysm). Aneurysms usually grow insidiously and cause no symptoms. The biggest danger is that the balloon bursts (ruptures). This can lead to severe internal bleeding, which can be fatal without immediate intervention. For this reason, aneurysms should be treated when they reach a certain diameter before the risk of rupture increases. There are two main approaches to treatment: open surgery to replace the aneurysm with a synthetic vessel or insertion of a stent-graft (EVAR/TEVAR) into the aneurysm through the groin.
Aortic dissection is much more sudden and dangerous. A small tear develops in the inner wall of the vessel and blood enters between the layers of the vessel wall through this tear and tears it apart. This can block the mouth of the vessels leading to vital organs such as the brain, heart and kidneys, or cause the vessel to rupture completely. Dissections (Type A), especially those involving the aorta (ascending aorta) coming out of the heart, require absolute surgical urgency and the patient must be operated on immediately. In the operation, the section of the aorta where the tear is located is removed and replaced with a synthetic vascular graft.
What are the Treatment Options for Advanced Heart Failure?
Heart failure is an end-stage condition in which the heart becomes fatigued over time due to coronary artery disease, valvular disease or high blood pressure and is unable to pump enough blood to meet the body’s needs. Modern medicine offers new hope to patients at a point where drug treatments are no longer sufficient.
The first of these options is “ventricular assist devices” or heart pumps. These devices, commonly known as LVADs, are mechanical pumps that take over the pumping task of a weakened heart. The device is connected at one end to the left ventricle of the heart and at the other end to the aorta, taking blood from the heart and pumping it directly into the body. These devices can act as a “bridge to transplant” for patients waiting for a heart transplant, or as a permanent solution (“destination therapy”) for elderly patients who are not eligible for transplant. Thanks to this technology, many patients who previously had no chance of survival can return to an active life.
The most definitive and ideal treatment for advanced heart failure is “heart transplantation”. In suitable patients, the patient’s own diseased heart is removed and replaced with a healthy heart from a brain-dead donor. Heart transplantation is a second chance at life, offering patients a normal or near-normal quality of life. However, post-transplant patients need to use immunosuppressive drugs for life to prevent the body from rejecting the new organ and should keep regular check-ups.
What Lifestyle Changes Can Be Made to Protect the Circulatory System?
All these high-tech treatments offered by modern medicine are of course very valuable. However, it is important to remember that the best treatment is prevention. It is up to us to maintain the health of our circulatory system and reduce the risk of such serious problems in the future. Simple steps can make a big difference.
Paying attention to your diet is the first and most important step. Enriching your table with fresh and natural foods, such as the Mediterranean diet, is the best thing you can do for your arteries.
Some recommended food groups:
- Green leafy vegetables (spinach, chard, arugula)
- Colored fruits (berries, pomegranates, citrus fruits)
- Whole grains (oats, bulgur, whole wheat bread)
- Legumes (lentils, chickpeas, beans)
- Fish containing healthy fats (salmon, sardines)
- Nuts such as walnuts and almonds
- Olive Oil
Here’s what you should avoid or limit:
- All packaged and processed foods
- Sugary drinks and ready-to-drink juices
- Excess salt and salty foods
- Solid and trans fats (margarine, fast-food products)
- Excessive consumption of red meat
- Pastries and white bakery products
In addition to diet, regular physical activity keeps blood vessels flexible and keeps blood pressure and weight under control. Even brisk walking for at least 30 minutes most days of the week can work wonders. Eliminating cigarettes from your life is the biggest favor you can do for your blood vessels. Smoking directly damages the arterial wall, incredibly accelerating the process of atherosclerosis. Finally, learning to manage stress is also critical for heart health. Yoga, meditation, engaging in a favorite hobby or simply spending time in nature will be good for both your soul and your heart. A healthy lifestyle is your most powerful medicine.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.