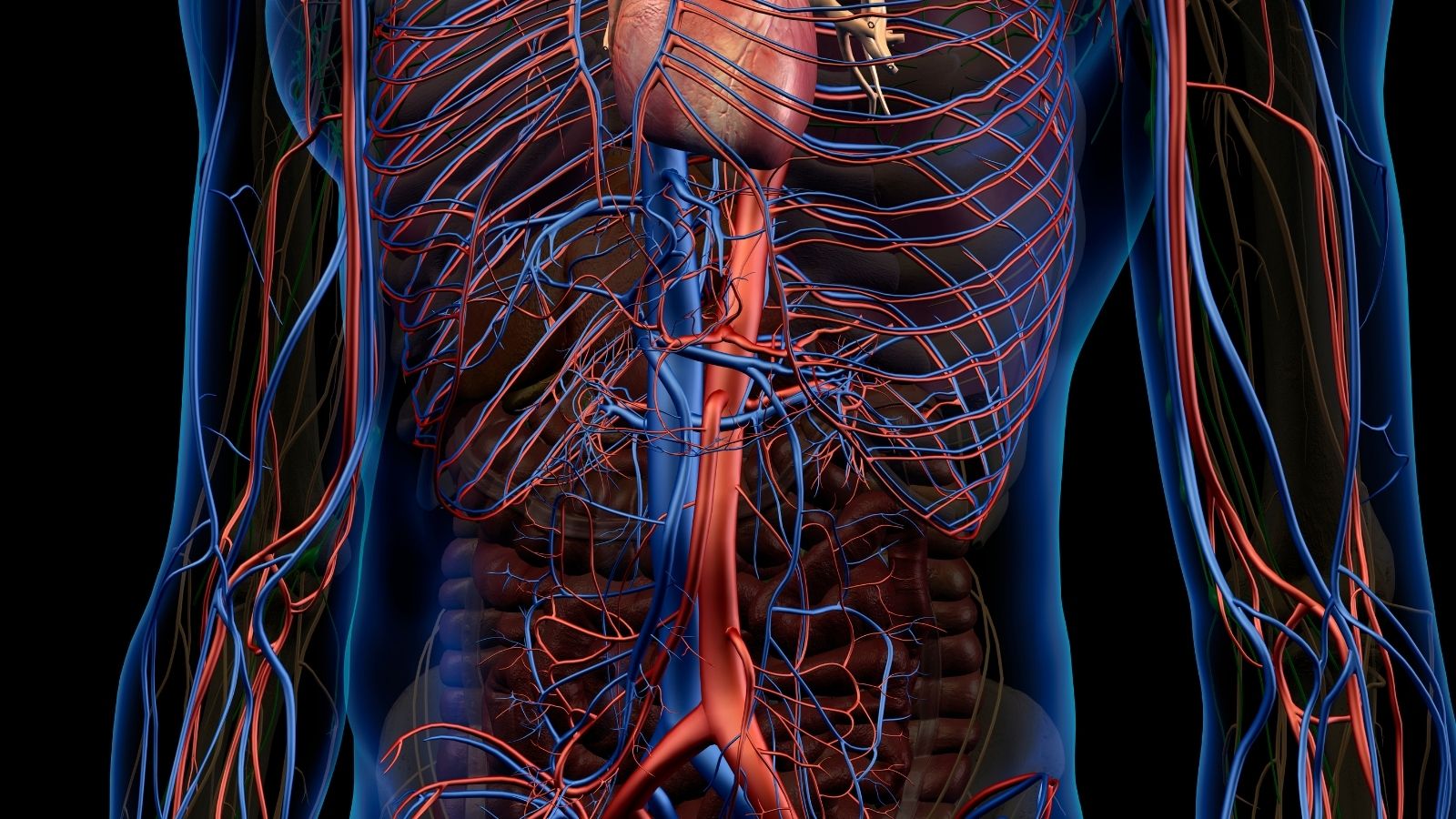
Infective aortitis is a rare but serious condition caused by bacterial infection of the aortic wall. It weakens the vessel, leading to aneurysm or rupture risk. The disease often arises from bacteremia, endocarditis, or direct extension of infection.
Common pathogens include Staphylococcus aureus, Salmonella species, and Streptococcus. Immunocompromised patients and those with prosthetic vascular grafts are at higher risk. Blood cultures are crucial for identifying the causative organism.
Diagnostic evaluation involves imaging techniques such as CT angiography and MRI to assess aortic involvement. Findings typically reveal wall thickening, irregularity, and periaortic inflammation. Prompt diagnosis is vital to prevent catastrophic complications.
Treatment requires prolonged intravenous antibiotic therapy combined with surgical repair in most cases. Aortic replacement with graft material is often necessary to restore vascular integrity. Delay in management significantly increases morbidity and mortality.
| Definition | Inflammation of the aortic wall due to infection |
| Causing Factors | Bacteria (especially Salmonella spp., Staphylococcus aureus, Streptococcus pneumoniae), rarely fungi |
| Risk Factors | Atherosclerosis, immunosuppression, diabetes mellitus, invasive procedures, bacteremia |
| Symptoms | Fever, chest/abdominal/back pain, weight loss, weakness, septic picture |
| Diagnostic Methods | Blood cultures, CT angiography, magnetic resonance imaging (MRI), PET-CT |
| Complications | Aortic aneurysm, rupture, sepsis, thrombosis, distal embolization |
| Treatment Methods | Antibiotic therapy (long-term, usually IV), surgical resection and reconstruction with graft |
| Follow-up and Monitoring | Infection control with blood cultures, evaluation of aortal structure with imaging |
| Ways of Prevention | Control of infection sources, sterile technique in invasive procedures, protection of the immune system |
What is Infective Aortitis and how does it so dangerously affect the body’s main artery?
Infective aortitis is a life-threatening infection that occurs when a microbe invades the wall of the aorta, the main artery of our body. The aorta can be likened to the main water pipe that carries water to all the houses in the city. The stronger this pipe is, the safer the system is. Infective aortitis is like a leak and the beginning of decay in the wall of this main tube.
The real danger of the disease comes not only from the infection itself, but also from the physical damage it causes to the aortic wall. When bacteria settle on the aortic wall, our body naturally sends defense cells to the area to fight them. But during this battle, powerful enzymes are released that break down the basic building blocks, such as collagen and elastin, which hold the vessel wall together and give it elasticity.
As a result, the aortic wall suddenly becomes weak, thinner and unable to withstand the high blood pressure inside it. This can lead to a dangerous ballooning of the vessel (aneurysm), a paper-like tearing of the wall layers (dissection) or, in the worst case scenario, a complete rupture (rupture). Therefore, infective aortitis should not be seen as an infection that can be treated with antibiotics alone. This is a loss of structural integrity in one of the body’s most important infrastructural systems that requires urgent intervention, which explains why surgical intervention is so critical.
What are the main differences between infective aortitis and non-infectious aortitis?
“Aortitis”, inflammation of the aortic wall, is a general definition and is basically divided into two main groups. Differentiating between these two conditions is an absolute must in order to choose the right treatment and save the patient’s life. Because what is good for one person can be disastrous for another.
Non-infectious aortitis is usually caused by autoimmune or rheumatic diseases in which the body’s own immune system attacks the aortic wall in surprise. In cases such as Giant Cell Arteritis or Takayasu Arteritis, the problem is internal; the body’s own defense system has locked onto the wrong target. In this case, treatment is aimed at calming this overreactive immune system with drugs such as cortisone.
Infective aortitis, on the contrary, is an active infection caused by an external enemy – bacteria or fungi. In this case, suppressing the immune system is tantamount to opening the door wide open to the enemy. The mainstay of treatment is high-dose antibiotics to destroy the germ and surgical removal of the damaged tissue that is the source of the infection.
The main features of these two situations are the following:
Infective Aortitis
- Cause: Direct attack by a microbe such as bacteria or fungus.
- Common Causes: Staphylococcus, Salmonella, Streptococcus.
- Progression: Usually very fast and devastating.
- Treatment: Antibiotics and emergency surgery.
- Main Hazard: Uncontrolled infection (sepsis) and sudden vessel rupture (rupture).
Non-infectious Aortitis
- Cause: Failure of the body’s own immune system (autoimmune).
- Common Causes: Giant Cell Arteritis, Takayasu Arteritis.
- Progression: Usually slower and chronic.
- Treatment: Immunosuppressive drugs (corticosteroids).
- Main Danger: An aneurysm or blockage of a blood vessel that develops slowly over the years.
How does the infection settle in the aortic wall and initiate the process of Infective Aortitis?
A healthy aortic wall has a natural armor against infections thanks to its smooth inner surface. Infective aortitis occurs when this armor is breached. We can think of it as a disease of “frailty”, meaning that the infection often settles into a pre-existing weakness.
We can think of the process as a two-step scenario. The first step is damage to the aortic wall. The most common cause is atherosclerosis, also known as arteriosclerosis. Over the years, cholesterol plaques build up, making the inner surface of the aorta rough and bumpy. These damaged surfaces are the perfect breeding ground for bacteria to take hold.
The second step is for the bacteria to somehow enter the bloodstream. This could be after a dental treatment, a urinary tract infection, a skin wound or a more serious infection. As it travels through the body, these bacteria “stick” to the previously damaged rough area in the aorta, where it establishes a colony and begins to multiply.
Once the bacteria become established, the body’s defense mechanisms kick in and an intense inflammatory response begins. But during this battle, the defense cells attacking the area, while trying to destroy the bacteria, also release powerful digestive enzymes that dissolve the structural proteins of the aortic wall. This “friendly fire” causes the aortic wall to rapidly weaken, thin and eventually expand like a sac (saccular aneurysm), ready to rupture.
Which bacterial species most commonly cause infective aortitis?
Although many different microbes can be behind cases of infective aortitis, some are more common in causing this dangerous condition. The most common culprits are:
- Staphylococcus species (especially Staphylococcus aureus)
- Salmonella species
- Streptococcus species (especially Streptococcus pneumoniae, which causes pneumonia)
- Enterococcus
- Escherichia coli (E. coli)
Who is at risk of developing Infective Aortitis?
Infective aortitis is often a “perfect storm” scenario caused by a combination of risk factors. It is very rare for it to develop in a healthy, young aorta. The main conditions that increase the risk are:
- Pre-existing aortic disease (most important factor)
- Arteriosclerosis (atherosclerosis)
- An existing aortic aneurysm
- Advanced age (usually over 50 years)
- A weakened immune system
- Diabetes (diabetes)
- Chronic alcoholism
- Diseases such as cancer or HIV
- Use of immunosuppressive drugs
- Intravenous drug use
- Previous aortic surgeries (open or closed)
- Vascular catheters that remain in the body for a long time
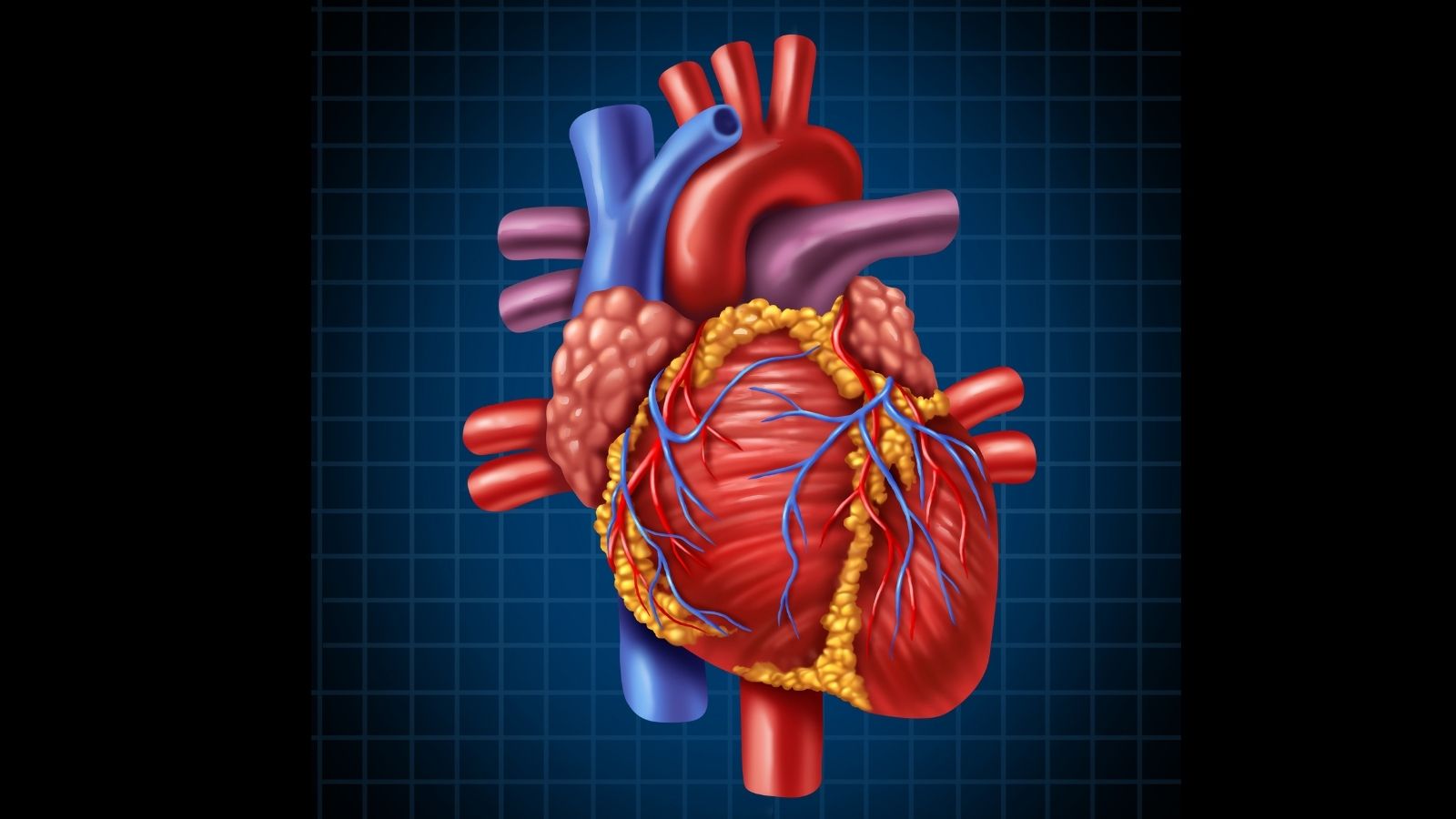
- Heart valve infection (infective endocarditis)
What are the symptoms that may indicate the presence of infective aortitis?
One of the most deceptive aspects of infective aortitis is that its symptoms are often very vague and can be confused with many common illnesses such as influenza, a herniated disc or a simple urinary tract infection. This can lead to a delayed diagnosis and waste valuable time. The main symptoms that patients should watch out for are:
- Stubborn fever that lasts for days or even weeks
- Trembling attacks
- Back, chest or abdominal pain that is constant or comes and goes
- Unexplained general weakness and fatigue
- Loss of appetite
- Unwanted weight loss
The triad of fever, abdominal pain and a palpable pulsating mass in the abdomen (pulsatile mass) described in the literature are actually found together in a very small number of patients. Therefore, if a person at risk has persistent fever and pain, this rare but serious possibility should be considered.
What tests do doctors use to confirm the diagnosis of Infective Aortitis?
The diagnosis of infective aortitis is not made by a single test, but by putting together a series of findings, like putting the pieces of a puzzle together. The main methods we use in this process are the following:
- Blood Cultures: This is our most valuable test to name the microbe causing the infection and determine which antibiotic will work.
- Inflammation Markers: Elevated values in the blood, such as CRP and sedimentation (ESR), indicate that there is inflammation in the body, but not where.
- White Blood Cell Count: An increase in leukocytes is another sign of an active infection.
- Tissue Biopsy: Examination of the diseased aortic tissue removed during surgery in the pathology laboratory is the “gold standard” method that confirms the diagnosis.
What is the role of imaging modalities such as CT, MRI and PET/CT in the diagnosis of infective aortitis?
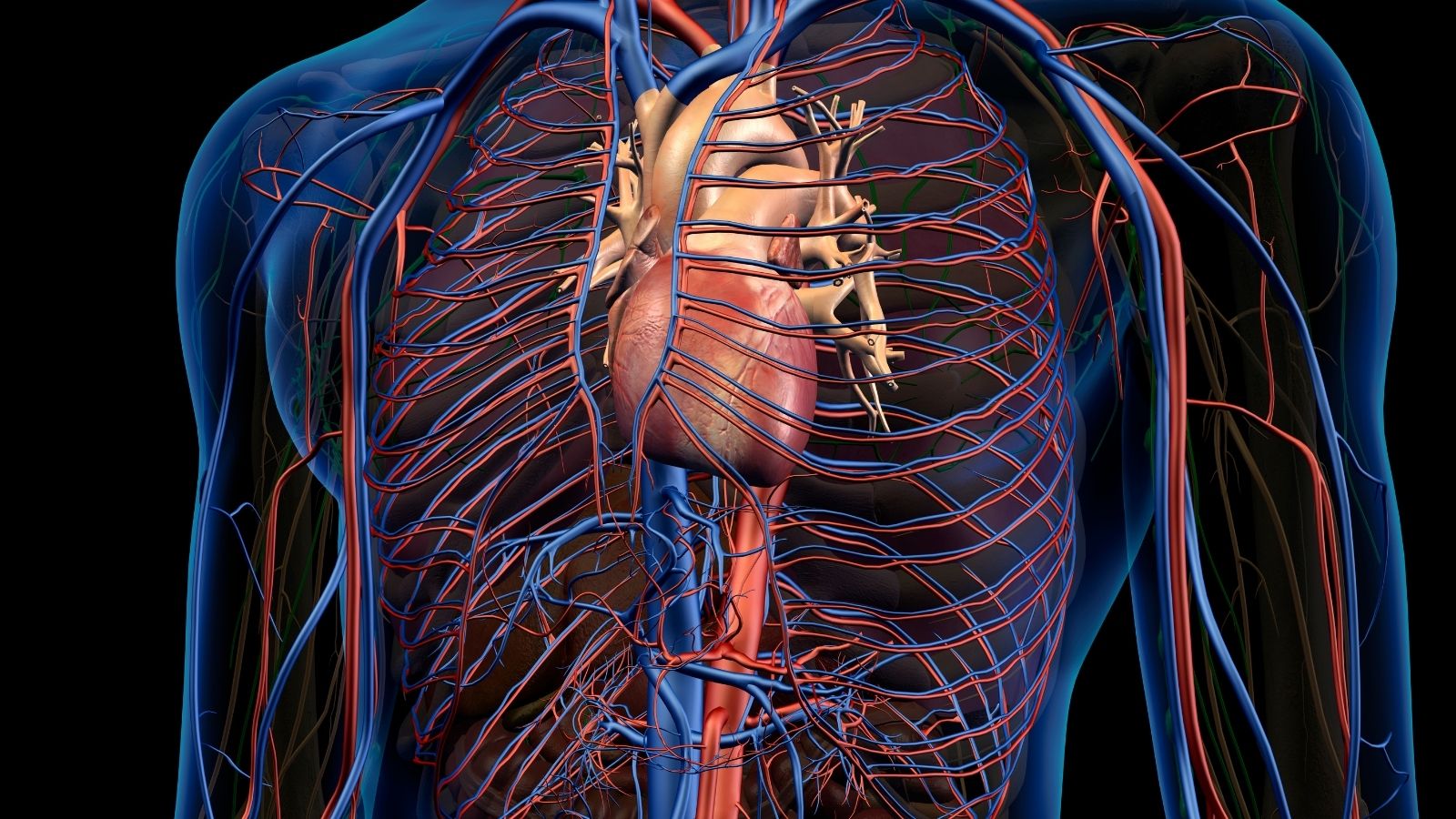
While laboratory tests tell us there is a problem, imaging methods show where and how big the problem is. They are therefore an indispensable part of the diagnostic process.
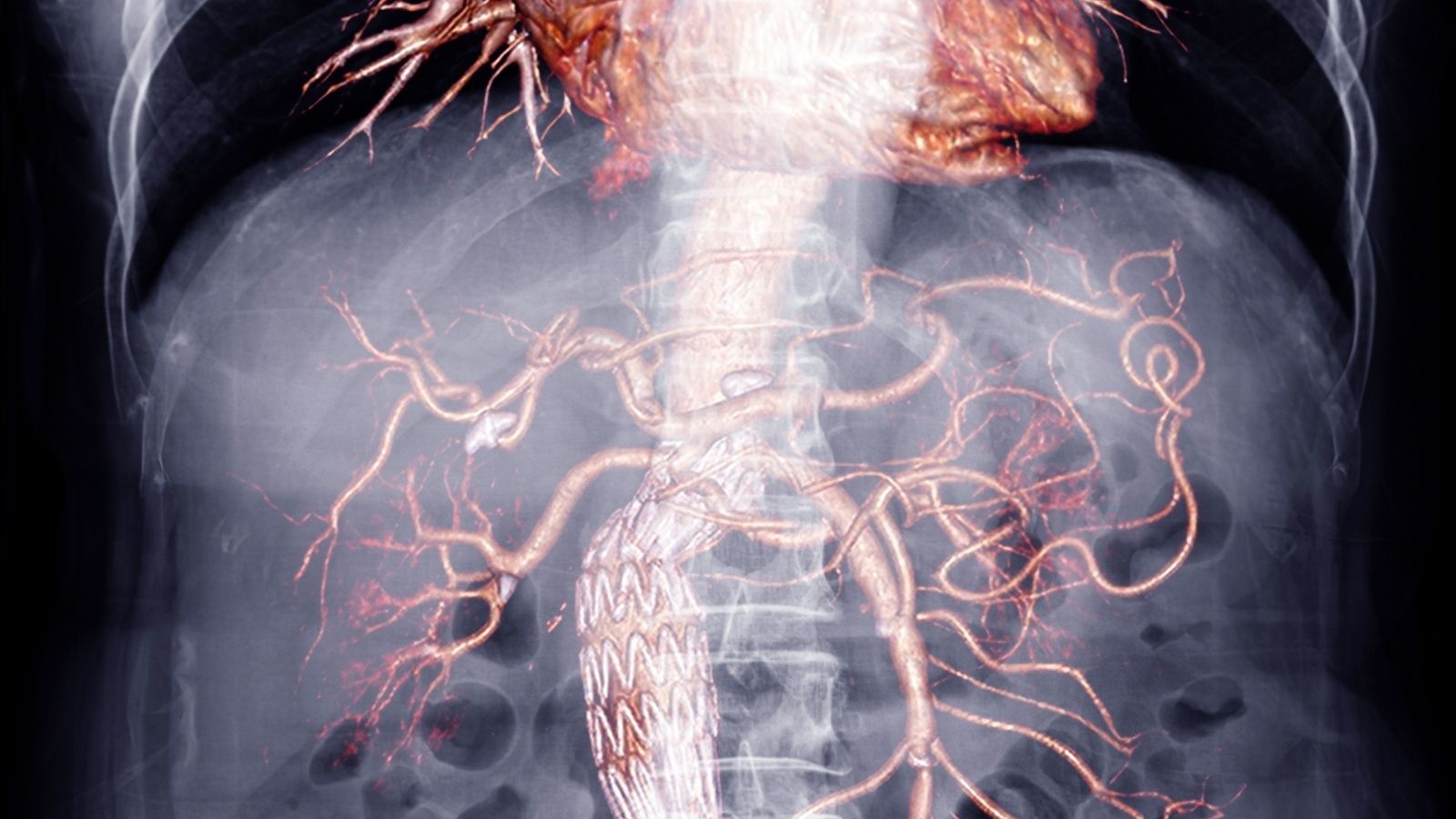
- Computed Tomography Angiography (CTA) is usually our first choice. It provides a three-dimensional map of the aorta by injecting contrast material through the vessel. With CTA, we can see thickening of the aortic wall, inflammation around it, sac-shaped aneurysms caused by infection, and sometimes even air bubbles that prove infection.
- Magnetic Resonance Angiography (MRA) is an excellent alternative, especially for patients with sensitive kidney function, as it is radiation-free. It is very successful in showing edema and active inflammation in the aortic wall.
- 18F-FDG Positron Emission Tomography (PET/CT) is one of the most exciting developments in this field. This technology detects metabolically active cells in the body, i.e. inflammatory cells that work hard, such as cancer cells. Inflammatory cells gathering at the site of infection appear as a bright “hot spot” on a PET/CT scan because they consume high amounts of sugar. The great power of PET/CT is that it can catch inflammation at a much earlier stage, before structural damage (such as an aneurysm) can be seen on a CT scan. This is a tremendous advantage to start treatment early and prevent fatal complications.
Why is Infective Aortitis caused by Staphylococcus aureus particularly dangerous?
If infective aortitis had a “personality”, the type caused by Staphylococcus aureus would be the most aggressive and unpredictable. Infection with this bacterium is usually treated as a medical emergency. This is because it progresses extremely quickly and can rupture the aortic wall, leading to fatal consequences such as rupture, even very soon after diagnosis. Patients’ condition can deteriorate rapidly within hours or days, despite receiving the right antibiotic treatment. This rapid destruction is a testament to how efficiently S. aureus produces enzymes that dissolve the aortic wall. Therefore, when this bacterium is suspected, it should be known that there is a race against time and both medical and surgical treatment should be started as soon as possible.
What are the salient features of Infective Aortitis caused by Salmonella bacteria?
Salmonella-induced aortitis, the “sleeping agent” of the disease as aortic infection. The most interesting feature of this species is that the aortic infection usually occurs following an episode of diarrhea (food poisoning) that occurred weeks or months ago and has been completely forgotten.
The mechanism behind this is quite insidious. Salmonella bacteria, which enter the bloodstream during an intestinal infection, can hide inside atherosclerotic plaques and wait quietly there for months or even years. Then, at a time of low body resistance, it reactivates and starts a destructive infection of the aortic wall. This “sleeping agent” nature makes diagnosis very difficult. Because by the time symptoms such as fever and back pain appear, the initial intestinal infection may have already been forgotten. Therefore, especially if a person with risk factors has a history of Salmonella-induced diarrhea, the suspicion of aortitis becomes even more important.
How is Streptococcus-induced Infective Aortitis diagnosed and treated?
Aortitis, especially that caused by Streptococcus pneumoniae, a known causative agent of pneumonia, usually has a more insidious onset and may take longer to diagnose. The most important lesson from the management of such infections is that antibiotic therapy alone is almost never sufficient. Clinical experience has repeatedly shown that despite appropriate antibiotic therapy, the disease continues to progress and the condition of patients without timely surgical intervention worsens. This proves that completely removing infected and structurally weakened aortic tissue and restoring vascular integrity is not an option but a necessity.
Why is both antibiotic therapy and surgical intervention often necessary in the treatment of infective aortitis?
The treatment of infective aortitis can be likened to treating a building that is on fire and the load-bearing columns are cracked. There are two things to do in this situation: first call the fire brigade to put out the fire, and then call the engineers and construction team to repair the damaged columns and save the building from collapse. Doing only one will result in disaster.
- Antibiotic Therapy (Fire Brigade): Its purpose is to extinguish the “fire” by removing bacteria from the bloodstream and prevent the infection from spreading to other organs (sepsis).
- Surgical Intervention (Construction and Demolition Team): Its purpose is to completely scrape out the damaged, infected and dead aortic tissue that is the main source of infection (demolishing the decayed parts of the building) and, most importantly, to replace the weakened aortic section with a strong artificial vessel (graft) (rebuilding the load-bearing columns of the building) to restore the structural integrity of the vessel and prevent rupture.
Proceeding with antibiotic treatment alone, i.e. simply putting out the fire and leaving the building alone, will eventually cause the already weakened walls of the structure to collapse. Therefore, a combination of medical and surgical treatment is the standard and most effective way to treat this disease.
Is Endovascular Repair (EVAR/TEVAR) a minimally invasive alternative for the treatment of Infective Aortitis?
Endovascular repair, the insertion of a stent-graft into the aneurysm through a small incision in the groin, has revolutionized the treatment of aortic diseases in recent years. However, its use in the treatment of infective aortitis is highly controversial. Because one of the basic surgical principles is to “never place a foreign body into an infected area” Endovascular repair violates this rule by doing this, that is, by placing a stent-graft into the infected aorta without clearing it.
Despite this, endovascular repair has a role in this disease. It may be an option, especially in patients who are too old, too frail or too seriously ill to tolerate open surgery. It can also be used as a life-saving “bridging” or “damage control” maneuver to rapidly control bleeding in a shocked patient with a ruptured aneurysm and bleeding. This allows the patient to plan a more permanent solution after stabilization. However, this is a carefully chosen approach that usually requires the patient to be on antibiotics for life and to be followed very closely.
What life-threatening complications can develop if infective aortitis is not treated?
If the infection is not controlled, it can lead to a series of catastrophes affecting the whole body, starting with the aorta. The main fatal complications that can develop are:
- Aortic rupture (tear)
- Sepsis (blood poisoning)
- Septic embolism (infected clots thrown into organs such as the brain and kidneys)
- Paralysis (stroke)
- Kidney failure
- Loss of limb
- Aortoenteric fistula (opening of the aorta into the intestine and bleeding into the digestive tract)
What is the prognosis and survival rate of a patient diagnosed with infective aortitis?
Unfortunately, the prognosis of infective aortitis, i.e. the prognosis for the course of the disease, is quite serious. Left untreated, the disease is almost always fatal. Even in patients who are diagnosed and treated, mortality rates are still high, depending on how early the diagnosis was made and whether complications develop.
But despite this bleak picture, there is hope. The most important factor determining survival is winning the race against time. Early diagnosis and urgent, appropriate treatment can completely change the prognosis. In particular, effective antibiotic therapy initiated at the time of suspicion and timely surgical intervention have been proven to significantly increase survival rates. This highlights how vital it is for the patient to reach a specialist center that can diagnose and manage this rare condition as soon as symptoms appear.
What kind of a long-term follow-up process awaits patients after treatment of infective aortitis?
Treatment of infective aortitis does not end with a successful surgery and a course of antibiotics. Rather, it is the beginning of a lifelong partnership between the patient and the aortic care team. The disease itself or the underlying vascular weakness puts the patient at risk of developing new problems in the future. Close and regular follow-up is therefore essential. This follow-up process includes:
- Regular imaging (CT or MR angiography)
- Monitoring inflammation markers with blood tests
- Strict control of blood pressure
- Good management of underlying diseases such as diabetes
- Immediate treatment of any new signs of infection (dental abscess, urinary tract infection, etc.)
This follow-up is done to check the condition of the implanted graft and, most importantly, to detect at an early stage whether a new aneurysm or inflammation has developed in another part of the aorta. This is an ongoing responsibility to protect the patient’s long-term health.
Frequently Asked Questions
What is infective aortitis?
Inflammation of the aorta caused by infection. It is a rare but serious life-threatening vascular disease.
What organisms are involved in this infection?
Bacteria such as Staphylococcus aureus, Salmonella species and Treponema pallidum are usually responsible.
How is it transmitted?
Infections that spread through the blood can settle in the aortic wall. It is especially common in people with weak immunity.
Who is at risk?
The elderly, people with weakened immune systems, those with chronic diseases and intravenous drug users are at risk.
What are the symptoms?
Fever, chest or back pain, weakness, weight loss and sometimes sepsis symptoms may occur.
How is it diagnosed?
Diagnosis is based on CT or MR angiography, blood cultures and laboratory tests.
Does it cause aortic aneurysm?
Yes, infection can weaken the aortic wall and cause an aneurysm to form.
What happens if left untreated?
Spread of infection can result in aortic rupture, sepsis and death.
How is it treated?
Start with broad-spectrum antibiotic treatment; sometimes surgical intervention may be required.
When is surgery performed?
Surgery is necessary in cases of aneurysm, risk of rupture or failure to respond to antibiotics.
How long is the treatment period?
Antibiotic treatment usually lasts 4-6 weeks, but can be extended depending on the situation.
Is this disease contagious?
It is not directly contagious, but underlying infections can be passed from person to person.
Is infective aortitis fatal?
Yes, it has a high mortality rate, especially in late diagnosed and untreated cases.
Which specialists treat?
Infectious diseases, cardiovascular surgery and radiology specialists plan treatment together.
Are there ways of prevention?
It is necessary to observe hygiene rules, strengthen the immune system and do not neglect the treatment of chronic infections.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.