The heart functions as a muscular pump that circulates blood throughout the body. It consists of four chambers and valves that regulate flow, ensuring oxygen-rich blood reaches tissues while oxygen-poor blood is sent to the lungs for reoxygenation.
The right atrium receives venous blood and transfers it to the right ventricle, which pumps it into the lungs. Here, carbon dioxide is exchanged for oxygen, allowing the blood to be enriched with vital gases before entering systemic circulation.
The left atrium receives oxygenated blood from the lungs and passes it into the left ventricle. As the most powerful chamber, the left ventricle pumps blood into the aorta under high pressure, ensuring distribution to all organs and tissues.
Valves between chambers maintain one-way flow, preventing backflow and maintaining efficiency. The coordinated contraction of atria and ventricles, regulated by the electrical conduction system, guarantees a steady rhythm and effective circulation.
What is the heart and where is it located in the body?
The answer to the question of where the heart is, which is frequently wondered by patients, is actually quite central. Contrary to popular belief, the heart is not located on the left side of the body, but in the center of the chest, just behind the breastbone. Only the tip is slightly turned to the left, so we feel its beating mostly on the left side. This muscular organ, which is about the size of each person’s own fist, is protected like armor by the rib cage along with the lungs. The most basic and vital function of the heart is to continuously distribute blood throughout the body like a pump. This provides our tissues and organs with the oxygen and nutrients they need to function.
What are the Layers that Make Up the Heart Wall?
The structure of the heart looks like a single muscle mass from the outside, but it is actually made up of three distinct and important layers. This structure, known as the layers of the heart, both protects the heart and keeps it functioning perfectly.
The wall of the heart is made up of three basic layers that protect it and make it work:
- Pericardium
- Myocardium
- Endocardium
The pericardium is a thin, double-layered membrane that surrounds the heart like an outer pouch. The slippery fluid between the layers of this membrane allows the heart to move freely and frictionlessly within the rib cage with each beat. It is the heart’s protective shield and lubrication system.
The myocardium is the middle layer of the heart and is its main engine. The thickest and strongest layer of the heart, the myocardium is a specialized muscle tissue responsible for the powerful contractions that pump blood to the lungs and throughout the body. In order for this muscle to work non-stop, it needs its own special feeding network, the coronary vessels.
The endocardium is like a smooth lining covering the innermost surface of the heart, its chambers and all its valves. This slippery surface allows the blood to flow through the heart without any roughness, sticking or clotting.
How Are the Chambers and Sections of the Heart Organized?
When we examine the internal structure of the heart, we see that it is a powerhouse with four chambers. These chambers, also known as the chambers of the heart or parts of the heart, direct the blood’s journey through the body. The heart is divided by a solid wall of muscle called the “septum” into a right side for oxygen-poor blood and a left side for oxygen-rich blood. Each side has an upper and a lower room.
The four main rooms of this power center are:
- Right Atrium (Right Atrium)
- Right Ventricle (Right Ventricle)
- Left Atrium (Left Atrium)
- Left Ventricle (Left Ventricle)
The atria, or atria, are like “reception chambers” at the top that collect blood. The right atrium collects dirty blood from the body and the left atrium collects clean blood from the lungs. The ventricles, or ventricles, are the larger, muscular “pump chambers” at the bottom. Blood passes from the atria to the ventricles, where it is pumped with great force. We notice that the wall of the left ventricle is much thicker than that of the right ventricle. This is because the right ventricle only sends blood to the nearby lungs, while the left ventricle has to generate much greater pressure to deliver the same blood throughout the body, from the brain to the toes, via the aorta.
What is the function of the heart valves and which ones are they?
Between the chambers of the heart and its main vessels, there are perfect structures that ensure that the blood flow always moves in the right direction and does not back up. These are the heart valves, which act like one-way doors. They regulate blood circulation by opening and closing in perfect timing with each heartbeat.
The heart has four vital valves that keep blood flowing in the right direction:
- Tricuspid Valve
- Pulmonary Valve
- Mitral Valve
- Aortic Valve
The tricuspid valve is located between the right atrium and the right ventricle. When the right ventricle contracts, this valve closes, preventing blood from escaping back into the right atrium. The pulmonary valve is between the right ventricle and the pulmonary artery and prevents blood from returning after being sent to the lungs. The mitral valve is located between the left atrium and the left ventricle and is the hardest working valve of the heart. It prevents blood from leaking into the left atrium during a strong contraction of the left ventricle. Finally, the aortic valve is located between the left ventricle and the aorta, the body’s main artery, and prevents clean blood from escaping back into the heart after being pumped throughout the body. Any problems with these valves can seriously increase the heart’s workload.
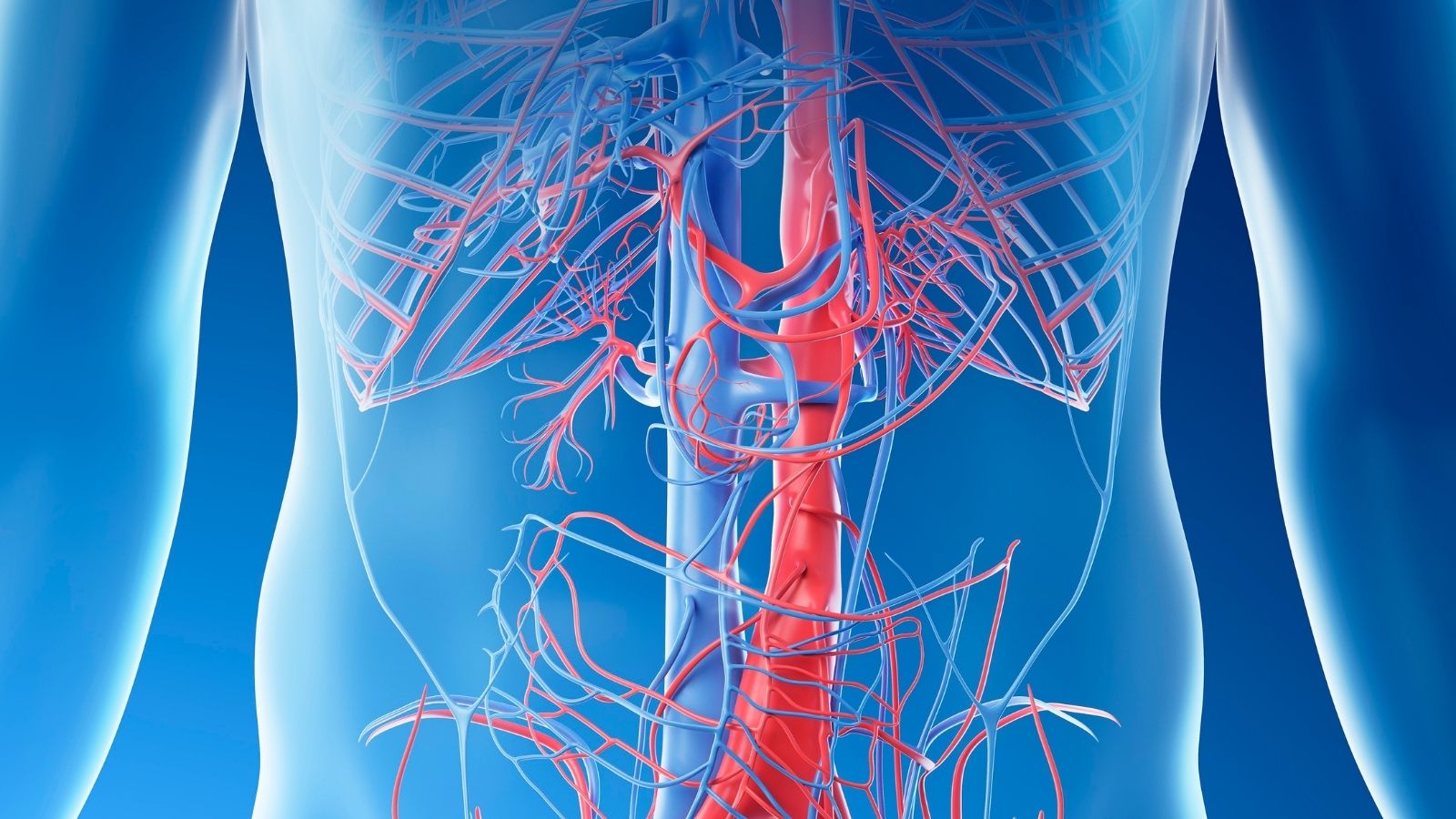
What are the main blood vessels entering and leaving the heart?
The heart is not an organ that works on its own. It is connected to large blood vessels that resemble the body’s highway network. The arteries (arteries) carry blood away from the heart, while the veins (veins) bring blood back to the heart.
The main arteries that take blood away from the heart are:
- Aorta
- Pulmonary Artery
The aorta is the largest and most important artery in the body, originating from the left ventricle. It is the main highway that distributes oxygen-rich blood to all organs and tissues. The pulmonary artery is an exception; it arises from the right ventricle and carries oxygen-poor blood to the lungs for purification.
The main veins that bring blood back to the heart are as follows
- Superior and Inferior Vena Cava
- Pulmonary Veins
The superior and inferior vena cava are two large veins that collect oxygen-poor blood from the upper and lower parts of the body and empty it into the right atrium of the heart. The pulmonary veins are an exception; they carry oxygen-rich blood that has been cleaned in the lungs to the left atrium of the heart.
What is the Cardiac Cycle and Where Do Heart Sounds Come From?
The cardiac cycle is the sequence of events that takes place when the heart fills with blood and pumps it once. It is the time from the beginning of one heartbeat to the beginning of the next. This rhythmic dance consists of two main periods: Diastole is when the heart relaxes and fills with blood. Systole is when the heart contracts and pumps this blood forward. At rest, this entire cycle takes less than a second.
So what is that famous “lub-dub, lub-dub, lub-dub” sound that doctors listen to with a stethoscope? These sounds come not from the blood itself, but from the closing of the valves, those one-way doors during the cardiac cycle. The first, fuller “LUB” sound is produced when the mitral and tricuspid valves close at the beginning of systole. The second, sharper “DUB” sound is heard at the end of systole when the aortic and pulmonary valves close. The rhythm, tone and presence of these sounds provide valuable clues about heart health.
How does blood travel through the heart and body?
The journey of blood through the body is a perfectly planned cycle that never stops. We can liken this journey to the route of a cargo vehicle. Let’s follow this route step by step:
The journey begins when “dirty” blood, which has been used and deoxygenated in the body, travels through two large veins (vena cava) to the right atrium (upper right chamber) of the heart. When this chamber is full, it contracts and sends blood to the right ventricle (lower right chamber) just below it.
The next stop is the lungs, the station for cleaning the blood. The right ventricle contracts strongly and pumps this dirty blood through the pulmonary artery to the lungs. In the lungs, the blood leaves the carbon dioxide waste it carries and is loaded with fresh oxygen as we breathe. It is now bright red, “clean” blood.
This clean blood, filled with oxygen, returns to the heart through the pulmonary veins and enters the left atrium (upper left chamber). When this chamber is full, it contracts and transfers blood to the left ventricle (lower left chamber), the strongest and most important chamber of the heart.
This is the big moment! The left ventricle contracts with tremendous force, ejecting this oxygen-rich blood into the aorta, the body’s main highway. Through smaller branches branching off from the aorta, blood delivers life-giving oxygen and nutrients from our brain to our fingertips and to all our organs and tissues.
Having completed its task, the blood releases oxygen into the tissues, collects waste, becomes polluted again and returns to the right side of the heart through the veins to start the endless cycle all over again.
How do the electrical signals that initiate a heartbeat occur?
What keeps the heart beating in a regular rhythm is its incredible electrical system. Just like the electrical wiring inside the walls of a house, the heart has a special network that gives the order to contract and transmits this order to the entire heart muscle. This system ensures that the atria (atria) and ventricles (ventricles) of the heart contract in perfect timing and in harmony with each other. This allows the heart to pump blood in the most efficient way. This electrical activity is so strong that it can be recorded by electrodes placed on the body surface (ECG).
What are the Parts of the Heart’s Electrical Wiring?
The main components of this ingenious electrical network are a central hub that initiates the stimulus and a network of wires that spreads it throughout the heart muscle.
The main components of this ingenious electrical network are:
- Sinoatrial (SA) Node
- Atrioventricular (AV) Node
- His Bundle
- Branch Bundles
- Purkinje Fibers
The Sinoatrial (SA) Node is the heart’s “natural battery” or “spark plug”. This small tissue, located in the upper part of the right atrium, spontaneously generates an electrical signal about 60 to 100 times per minute at rest and initiates the heartbeat.
The atrioventricular (AV) node is like a “junction” or “delay box” between the atria and ventricles. When the electrical signal from the SA node arrives here, it is deliberately delayed for much less than a second. This tiny delay is not a mistake but a marvel of design. This waiting period gives the atria time to complete their contractions and empty their blood into the ventricles.
After this short delay, the signal is rapidly transmitted through the bundle of His, the right and left bundles of branches and finally the Purkinje fibers, which spread like a network throughout the entire ventricular muscle. This propagation allows the ventricles to contract in a powerful and synchronized way, ejecting blood throughout the body and into the lungs. Any malfunction in this system can lead to rhythm disturbances (arrhythmias).
How the Heart Nourishes Itself and Why Coronary Arteries are Vital
While the heart pumps blood throughout the body, it also needs oxygen and nutrients. But how does it meet this need? This is where the coronary arteries, the heart’s own special “plumbing system”, come into play. These vessels are the first branches to leave the aorta and wrap around the surface of the heart like a crown, bringing oxygen-rich blood to the heart muscle (myocardium), which is working non-stop.
One of the most interesting features of this system is this: While all other organs in the body receive most of their blood flow when the heart is contracting (systole), the heart muscle receives most of its blood at the opposite time, when the heart is relaxing (diastole). This is because when the heart contracts, it squeezes these small vessels within itself, making blood flow temporarily difficult. When relaxed, these vessels relax and fill with blood.
This is why coronary artery disease, i.e. the narrowing or blockage of these vessels by calcification (atherosclerosis), is so dangerous. A narrowed artery cannot meet the increased oxygen demand of the heart muscle, especially during exertion (when the heart beats faster and relaxation time is shorter). This causes chest pain known as “angina”. If this blood vessel is suddenly completely blocked by a clot, the area of the heart muscle it supplies is damaged and this is called a heart attack (myocardial infarction).
How Our Body Adjusts Heart Rate According to Our Needs
Your heart does not always beat at the same speed. It slows down when you are sitting calmly and speeds up when you are running to catch a bus. This fine-tuning is managed by the autonomic nervous system and hormones according to the body’s instantaneous need for oxygen. This system works like the gas and brake pedals of a car.
This fine-tuning is managed by two opposing branches of the autonomic nervous system:
- Sympathetic Nervous System (Gas Pedal)
- Parasympathetic Nervous System (Brake Pedal)
The sympathetic nervous system is the “gas pedal” that governs our “fight or flight” response. It is activated in moments of exercise, stress, excitement or fear, increasing the heart rate and the contractile force of the heart. It prepares the body for challenging situations.
The parasympathetic nervous system is the “brake pedal” that governs the “rest and digest” mode. It is dominant when we are resting, sleeping or in our moments of calm and maintains energy by slowing down the heart rate.
The constant and dynamic balance between these two systems ensures that the heart performs optimally for the body’s needs at any given moment. For example, when you start exercising, first the “brake” (parasympathetic system) is slowly released, then the “throttle” (sympathetic system) kicks in to increase the speed even more. This is not a simple on-off switch but a highly sophisticated control mechanism.
What is coronary artery disease (plumbing problem) and what symptoms does it cause?
Coronary artery disease is a narrowing or blockage of the coronary arteries, the heart’s own “plumbing pipes”. This narrowing is caused by fatty deposits called “plaque” that build up on the vessel wall. Just as the flow of water is reduced when the plumbing pipe is lined with limescale, plaques make it difficult for blood to flow.
This is especially noticeable when the heart needs more blood. Some of the common symptoms include:
- Feeling of pressure, tightness or heaviness in the chest (angina)
- Shortness of breath (especially with exertion)
- Quick fatigue
- Chest pain radiating to the arm, shoulder, neck or jaw
A heart attack occurs when a plaque suddenly ruptures and the clot that forms on it completely blocks the blood vessel. The symptoms of a heart attack are more severe:
- Severe and prolonged chest pain
- Cold sweating
- Nausea and vomiting
- Dizziness and fainting
What are Heart Rhythm Disorders (Electrical Problems)?
Arrhythmias are malfunctions in the heart’s “electrical wiring”. It is a condition in which the heartbeat is faster, slower or irregular than normal.
Some of the most common rhythm disorders are as follows:
- Tachycardia (heart beating too fast)
- Bradycardia (the heart beats very slowly)
- Atrial Fibrillation (irregular and rapid pulsation of the atria)
- Extrasystoles (felt misfires or extra beats in the heart)
Among these rhythm disorders, Atrial Fibrillation (AFib) is particularly important. In this case, the atria cannot contract effectively and the blood can pool in the atria and form a clot. If this clot travels to the brain, it can result in a stroke.
What Does Heart Valve Diseases (Door Problem) Mean?
Valve disease is when the “doors” inside the heart do not work properly. These doors either fail to open fully, making it difficult for blood to pass through, or fail to close fully, causing blood to escape backwards.
Valve diseases basically occur in two ways:
- Stenosis (Stenosis)
- Insufficiency (Regurgitation or Leakage)
Stenosis is when the valve hardens and calcifies, restricting its opening. The heart has to work harder and harder to get blood through this narrow door and becomes tired over time. Insufficiency is when the valve fails to close completely and leaks blood backwards. In this case, the heart works inefficiently by having to pump the same blood over and over again, and over time it grows and loses its strength. Both conditions can lead to severe heart failure if left untreated.
Fortunately, medicine and technology offer highly effective solutions for the “plumbing”, “electrical” and “door” problems mentioned above.
What Treatment Methods Are There for Blocked Coronary Arteries?
There are several modern methods to open narrowed or blocked coronary arteries and restore blood supply to the heart muscle:
- Angioplasty and Stenting
- Coronary Artery Bypass Surgery (CABG)
In angioplasty and stenting, a thin wire is inserted into the vessel, usually through the groin or wrist, and a balloon is inflated to reach the blocked area and open the stenosis. A metal cage called a “stent” is usually inserted to prevent the vessel from closing again. Bypass surgery is an open heart surgery that is preferred for more multiple or complex vascular blockages. In this surgery, veins from another part of the body (from the chest, arm or leg) are used to create a new “bridge” or “bypass” to carry blood further away from the blockage.
What are the Modern Treatment Methods for Rhythm Disorders?
Treatment of rhythm disorders depends on the type and severity of the problem:
- Medication Therapy
- Electrical Cardioversion (Shock Therapy)
- Catheter Ablation
- Pacemaker or ICD (Shock Device)
- Surgical Ablation (Maze Procedure)
Medicines can help to regulate the rhythm or control the heart rate. Cardioversion is a controlled electric shock used to “reset” the heart. Catheter ablation is a procedure in which the foci of tissue that produce abnormal electrical signals that cause the arrhythmia are destroyed by burning or freezing them with special catheters inserted through the groin. A pacemaker may be implanted in cases where the heart beats very slowly, and an ICD (shock device) may be implanted in cases of life-threatening fast rhythms. The Maze procedure is a surgical ablation method usually performed during another heart surgery, especially to treat atrial fibrillation.
What Surgeries Are Performed for Deteriorating Heart Valves?
In advanced valvular disease, surgery is needed to relieve the heart and prolong life:
- Cover Repair (Repair)
- Valve Replacement
Whenever possible, especially for the mitral valve, repairing the patient’s own valve is the first choice. This is the ideal solution as it preserves the body’s own tissue. However, if the structure of the valve is not suitable for repair, the damaged valve is removed and replaced with a new prosthetic valve. The prostheses used in this replacement surgery can be mechanical (metal) or biological (from animal tissue). Which option is appropriate depends on the patient’s age, general condition and expectations.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.