Pacemaker surgery is performed to regulate abnormal heart rhythms by delivering electrical impulses. It is typically indicated in patients with bradycardia, conduction disorders, or heart block that impair cardiac function.
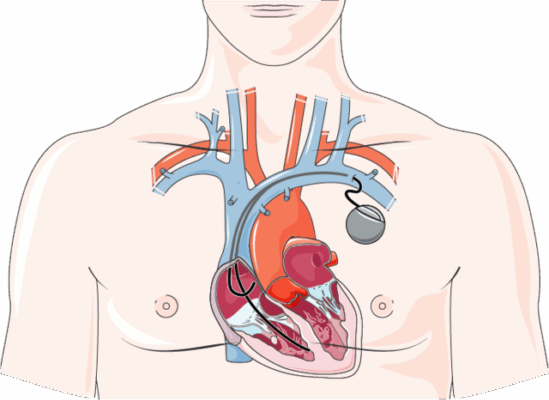
The implantation procedure involves placing a small device under the skin near the collarbone, with leads extending into the heart chambers. The device continuously monitors and corrects irregular rhythms, improving circulation efficiency.
Benefits of pacemaker implantation include reduced dizziness, fatigue, and syncope. Patients often experience improved quality of life, better exercise tolerance, and reduced risk of life-threatening arrhythmias.
Potential risks involve infection, lead displacement, or device malfunction. Regular follow-up and device checks are essential to ensure proper functioning and timely adjustments, securing long-term therapeutic success.
| Medical Name | Permanent Pacemaker Implantation |
| Type | Cardiac implant surgery |
| Affected System | Cardiovascular system (especially the electrical conduction system) |
| Indications | Symptomatic bradycardia, AV complete block, sinus node dysfunction, some cases of heart failure (CRT) |
| Objective | Regulate heart rate and prevent syncope, fatigue, congestive symptoms |
| Application Method | Placement of electrodes in the heart via the subclavian vein under local anesthesia; battery generator is implanted under the chest |
| Device Types | Single-chamber, dual-chamber, triple-chamber (CRT); some models include defibrillator (ICD) |
| Complications | Infection, electrode dislocation, hematoma, pneumothorax, battery life issues |
| Monitoring | Regular device checks, monitoring battery life, monitoring signs of infection, protection from magnetic fields |
What is a Pacemaker and How Does It Regulate the Heart’s Rhythm?
Our heart is a non-stop engine with a perfect electrical system within itself. The spark plug of this engine, the natural battery that starts the rhythm, is called the “sinoatrial node”. This natural battery regularly sends electrical signals to make the chambers of your heart contract in the correct sequence so that blood is pumped efficiently to every corner of your body. Sometimes, however, with age, a heart condition or certain medications, this natural pacemaker can weaken or interfere with the transmission of signals. This is when the heartbeat becomes dangerously slow (bradycardia) and your body does not get enough blood.
A pacemaker is a smart backup power source that comes into play at this point. This system basically consists of two parts. The first is a metal generator, slightly smaller than a matchbox, which contains a long-lasting battery and a computer chip that constantly listens to your heart. This generator is placed in a small pocket, usually under your collarbone, just under your skin. The second part is the thin, flexible, insulating wires called “electrodes” or “leads” that connect this generator to your heart. These cables are delivered through a vein to the chamber or chambers of your heart that need support, and the tip is gently secured to the heart muscle.
Modern pacemakers are not devices that put constant strain on your heart. Rather, they are “intelligent observers”. They listen continuously to your heart’s own rhythm and only kick in when it needs them. If your heart is beating at a normal rate, the battery waits passively. But the moment it senses that your heartbeat has fallen below a predetermined safe limit, it kicks in, sending electrical signals so small that you can’t feel them, returning your heart to its proper rhythm. Some advanced models even have sensors that can detect your body’s increased need for blood as you climb stairs or take a walk, safely increasing your heart rate to match your activity. In other words, a pacemaker doesn’t take away your heart’s work; it just gives it a helping hand when it needs it.
When is Pacemaker Surgery Necessary?
The decision for pacemaker surgery is made when your heart has become too slow to meet your body’s needs, or when you experience dangerous pauses between heartbeats. Installing a pacemaker in the heart is the most effective and permanent solution to eliminate the symptoms caused by these problems.
The most common medical reasons for pacemaker implantation are:
- Bradycardia (Abnormally Slow Heart Rate)
- Heart Block (Conduction Problems)
- Unexplained Fainting (Syncope)
- Specific Types of Heart Failure
- Making Other Treatments Safe
Let’s look at what these conditions mean. Bradycardia is when your heart beats slower than normal, even at rest. This can leave you feeling tired, short of breath and dizzy all the time. Heart block is a disruption in the highway of electrical signals between the upper and lower chambers of your heart; when the signals slow down or are completely interrupted, the heartbeat is severely slowed.
Sometimes the underlying cause of fainting spells is found to be a sudden stop in the heart. In this case, a pacemaker is used to prevent future fainting and related injuries. In some heart failure patients, the right and left ventricles of the heart cannot contract simultaneously. This incompatibility reduces the pumping power of the heart. Here, a special pacemaker called a “biventricular” pacemaker stimulates both ventricles at the same time, restoring this synchronization and improving heart function. Finally, sometimes medications used to control fast rhythm disorders such as atrial fibrillation can slow down the heart rate too much. In this case, the pacemaker acts as a “safety net”, allowing doctors to safely administer the necessary medications.
What Are the Traditional Types of Pacemakers?
Traditional pacemakers differ according to which part of your heart needs support. These pacemakers are classified according to the number of wires (electrodes) connected to the heart. There are basically three main types:
- Single-Chamber Pacemaker
- Dual-Chamber Pacemaker
- Biventricular Pacemaker (CRT/Tri-Polar)
Unipolar pacemakers are the most basic model and are connected to the heart by a single wire. It is usually placed in the lower chamber (ventricle) of the heart and stimulates only this chamber.
Bipolar batteries use two wires. One is placed in the upper chamber of the heart (atrium) and the other in the lower chamber (ventricle). The main advantage of this design is that it better mimics the natural way the heart works, that is, the upper and lower chambers contract in unison. This allows the heart to pump blood more efficiently.
Biventricular pacemakers (CRT) are the most advanced systems and use three wires. Two of these wires are placed on the right side of the heart like traditional pacemakers, while the third is positioned with a special technique to stimulate the lower left chamber of the heart (left ventricle). This pacemaker is specifically designed for patients with heart failure and an impaired timing of contractions between the right and left ventricles of the heart. Its purpose is to correct this mismatch, increasing the heart’s contractile force and pumping efficiency.
What is a Leadless Pacemaker and Who is it Suitable for?
The wireless pacemaker is a highly innovative technology that, as the name suggests, does not require the wires and surgical pockets in the chest of traditional pacemakers. This device is a self-contained miniature pacemaker, the size of a large vitamin capsule, and is implanted directly inside your heart.
Most of the long-term problems with traditional pacemaker therapy are related to the wires and the pocket in which the pacemaker is placed. The cables can become damaged or infected over time. Wireless technology has been developed to eliminate these problems. In a procedure similar to an angioplasty, the device is inserted through a vein in the groin, delivered to the lower right chamber of the heart and fixed there.
This modern approach has significant advantages:
- Reduced risk of complications (cable and pocket problems are eliminated)
- Better cosmetic result (no scarring or puffiness of the breast)
- Faster recovery (no postoperative arm restrictions required)
However, this technology is not yet suitable for every patient. Existing wireless batteries are currently generally only able to stimulate a single chamber of the heart (the right ventricle). They are therefore an ideal option for patients who only need this type of stimulation. For more complex rhythm problems, traditional systems are still the standard of care. Your doctor will decide which technology is best for you, depending on the type of heart rhythm problem you have and your general health.
What is the Preparation Process Before Pacemaker Surgery?
Preparation before pacemaker surgery is a team effort between you and our healthcare team to ensure that your procedure goes as safely and smoothly as possible. There are some important steps you should pay attention to in this process:
- Medicines Regulation
- Hunger Status
- Personal Preparation
- Companion Planning
One of the most critical steps in preparation is the management of your medications. In particular, blood thinners (aspirin, warfarin, Plavix, etc.) may need to be stopped a few days before the procedure under the supervision of a physician. After midnight the night before the operation, you will usually be asked to fast and dehydrate for at least 6-8 hours. This is a standard safety precaution to avoid possible risks during anesthesia. It makes the process easier if you wear comfortable clothes to the hospital and leave your accessories such as jewelry at home. Since you will not be able to drive after the procedure, it is imperative that you organize in advance the accompaniment of a relative who will drive you home.
How is Traditional Implantation Performed Step by Step?
One of the most frequently asked questions of our patients is “how long does pacemaker surgery take?”. Traditional pacemaker implantation is a highly controlled and painless procedure, usually performed under local anesthesia and completed in an average of one hour.
The procedure is performed in a specially equipped laboratory. First, a mild sedative is given through a vein in your arm to help you relax. This way you will not feel any anxiety or pain during the procedure, even if you are awake. Then, usually the area below your collarbone is completely numbed with a local anesthetic injection.
The surgeon makes a small incision in this anesthetized area, creating a pocket under the skin to house the battery generator. Then, guided by instant X-ray images, wires called electrodes are inserted through a vein near the incision site and delivered to the targeted chambers of your heart. The ends of the cables are gently secured to hold them securely to the heart muscle.
After the electrodes are implanted, their function is rigorously tested. During these tests, your heart is checked to see if it is responding correctly to the impulses. If all is well, the other ends of the wires are connected to the battery generator, which is inserted into the prepared subcutaneous pocket. Finally, the surgical incision is closed with sutures and covered with a sterile bandage.
How to Implant a Wireless Pacemaker?
Wireless pacemaker implantation is a minimally invasive procedure that does not require a surgical incision in your chest and is performed very similarly to an angioplasty procedure.
This modern procedure is performed in the patient’s groin area. After the procedure site is numbed with local anesthesia, the surgeon creates a small entry point into the large vein in the groin (femoral vein). Through this entry point, a thin, flexible catheter system containing a miniature pacemaker is inserted into the vein. Under the guidance of instant X-ray imaging, the surgeon carefully advances this catheter along the vascular system to the lower right chamber of the heart.
Once the catheter is in the correct position, the capsule-shaped wireless pacemaker is pushed out through the catheter and the tip is fixed to the inner surface of the heart wall. Once the device is secured, its functionality is tested. When all tests are successful, the catheter system is completely removed from the body and the small entry point in the groin is closed with a simple pressure bandage. This procedure, which usually takes less than an hour, offers a faster healing process than the traditional method.
What are the Possible Risks and Complications of Pacemaker Surgery?
One of the most natural concerns of our patients is “is pacemaker surgery risky?”. Pacemaker surgery is a routine procedure in modern medicine that is extremely safe and has a very high success rate. But like any surgical procedure, it involves some potential risks. Fortunately, serious complications are rare. We can analyze these risks in two groups.
Early risks that may occur during or immediately after the procedure include the following:
- Infection
- Bleeding or bruising (hematoma)
- Lung deflation (pneumothorax)
- Vascular or nerve damage
- Perforation of the heart wall (cardiac perforation)
The long-term risks that may develop over time with the use of the device are as follows:
- Cable (electrode) problems (displacement, breakage)
- Electronic malfunction of the device
- Abrasion of the skin over the battery (pocket erosion)
- Rotation of the device in the pocket (Twiddler syndrome)
Recognizing and managing these risks is the basis of patient safety. Thanks to the experience of the surgical team and the modern techniques used, the likelihood of these risks is very low. In particular, the risk of infection is minimized by sterile surgical conditions and prophylactic antibiotics. Very rare conditions such as perforation of the heart wall or lung deflation can be recognized and managed immediately by an experienced team. Long-term cable problems have been reduced thanks to durable cables produced with today’s technology. Remember that new technologies, such as wireless batteries, eliminate risks, especially cable and pocket issues.
What to Consider When Returning Home After Pacemaker Surgery?

The first few weeks after you return home are critical for your pacemaker’s wires to become firmly embedded and fused to the heart tissue. It is vital for the long-term success of your treatment that you follow certain activity restrictions during this period. The purpose of these restrictions is not to tire your heart, but to prevent the delicate new wires from moving out of place.
Things to consider when it comes to wound care:
- Keep the surgical incision dry and clean for the first 4-5 days.
- Do not apply lotion, cream or powder on the incision.
- If you notice signs of infection such as redness, swelling, discharge or fever, contact your doctor immediately.
Activity restrictions that usually apply for the first 4-8 weeks are as follows:
- Avoid raising your arm above shoulder level on the side where the battery is installed.
- do not lift objects weighing more than 4-5 kilograms.
- Avoid strenuous movements that require pushing and pulling (vacuuming, mowing the lawn).
- Avoid sports such as golf, tennis, swimming and activities that require contact.
What precautions should be taken in daily life?
For the most part, living with a pacemaker means returning to a normal and active life. Modern pacemakers are designed to be unaffected by most electronic devices we encounter in everyday life. However, it is useful to know some simple precautions.
Generally safe appliances are household appliances such as microwave ovens, televisions, computers and electric blankets.
Situations and devices to watch out for are:
- Cell phones
- Security systems and metal detectors
- Strong magnetic fields (welding machines, high voltage lines)
- Some medical procedures (MRI, diathermy)
When using your cell phone, as a precaution, it is advisable to hold it to your other ear instead of the side where your battery is inserted and not to carry it in your breast pocket. It is best to show your pacemaker ID card to the staff when going through security systems in places like airports. These systems will not damage your pacemaker, but they may raise an alarm because they contain metal. You should also inform your doctor that you have a pacemaker before any medical or dental treatment.
How Long is the Battery Life and How to Replace it?
One of the most common questions our patients ask is “how long does a pacemaker last?” and what happens when it expires. The battery of your pacemaker usually has a lifespan of between 7 and 15 years, depending on your frequency of use and the type of device.
It is not possible for the battery to die suddenly and without warning. The condition of your battery is determined months in advance during regular checks. In this way, battery replacement is organized as a planned and simple process, without an emergency.
the answer to the question “How long does a pacemaker replacement take?” is very short. This procedure is much simpler than the initial surgery and usually takes 30-45 minutes. Only the pacemaker generator is replaced; if the wires in your heart are working properly, they are not touched. The old generator is removed through the old incision and replaced with a new one. The healing process is also much faster than the first surgery.
Frequently Asked Questions
What is pacemaker surgery?
Pacemaker surgery is a surgical procedure in which a pacemaker device is implanted under the skin to regulate the electrical activity of the heart.
Who gets a pacemaker?
It is recommended for patients with a slow heart rhythm, heart block or certain types of arrhythmia.
How long does pacemaker surgery take?
It is a procedure that usually lasts between 1 and 2 hours and is performed under local anesthesia.
Is there pain after surgery?
Mild pain and swelling are normal and can usually be controlled with painkillers.
How long is the hospital stay after surgery?
Patients are usually discharged within 1-2 days.
How does a pacemaker work?
It monitors the heart’s beating rate and maintains a regular rhythm by sending electrical impulses when needed.
How long does a pacemaker last?
It usually lasts between 5-15 years; the battery is replaced before it runs out.
How is battery replacement surgery?
Only the generator part is replaced; the electrodes are usually left in place.
Can someone with a pacemaker return to their daily life?
Yes, most patients can return to normal life within a few weeks.
Are pacemakers compatible with MRI devices?
New generation batteries are MRI compatible; doctor’s approval is still required.
Can pacemakers use cell phones or microwaves?
Yes, but electronic devices should be kept away from the battery.
Can I exercise after a pacemaker implantation?
Light exercise is usually appropriate; it should be done with the doctor’s approval.
What to do if a pacemaker becomes infected?
The infected battery is removed and a new battery is inserted after the infection has been treated.
Does a pacemaker cause problems at airport control?
May interfere with metal detectors; carry a battery card and inform the staff.
Does a person with a pacemaker live longer?
Improves quality of life by regulating heart rhythm and reduces the risk of sudden cardiac arrest.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.