A penetrating aortic ulcer is a vascular pathology where an atherosclerotic plaque erodes the inner lining of the aortic wall, penetrating into deeper layers. This condition can progress to intramural hematoma, dissection, or rupture if untreated.
Symptoms of penetrating aortic ulcer often include sudden, severe chest or back pain. In many cases, the clinical presentation resembles aortic dissection, which makes advanced imaging such as CT angiography essential for accurate diagnosis.
Risk factors for penetrating aortic ulcer include longstanding hypertension, advanced age, smoking, and severe atherosclerosis. These conditions weaken the aortic wall, increasing susceptibility to ulcer formation and progression.
Treatment depends on ulcer size and clinical stability. While small, asymptomatic ulcers may be managed conservatively with blood pressure control, larger or complicated cases require endovascular repair or surgical intervention to prevent fatal outcomes.
| Definition | A condition in which atherosclerotic plaques in the aortic wall cause ulceration and perforation of the inner layer |
| Causing Factors | Atherosclerosis, hypertension, weakening of vascular structure associated with aging |
| Risk Factors | Advanced age, hypertension, smoking, hyperlipidemia, coronary artery disease |
| Symptoms | Sudden onset of chest or back pain, often similar to dissection; may be asymptomatic |
| Diagnostic Methods | CT angiography (most sensitive method), MRI, transesophageal echocardiography (TEE) |
| Complications | Aortic dissection, intramural hematoma, aortic rupture, tamponade |
| Treatment Methods | Conservative treatment and close follow-up in asymptomatic small lesions; endovascular (TEVAR) or surgical intervention in symptomatic or complicated cases |
| Follow-up and Monitoring | Lesion monitoring with regular CT/MRI controls, control of cardiovascular risk factors |
| Ways of Prevention | Atherosclerosis prevention, blood pressure regulation, smoking cessation, regular cardiological monitoring |
What is Penetrating Aortic Ulcer and What is its Place Among Other Aortic Diseases?
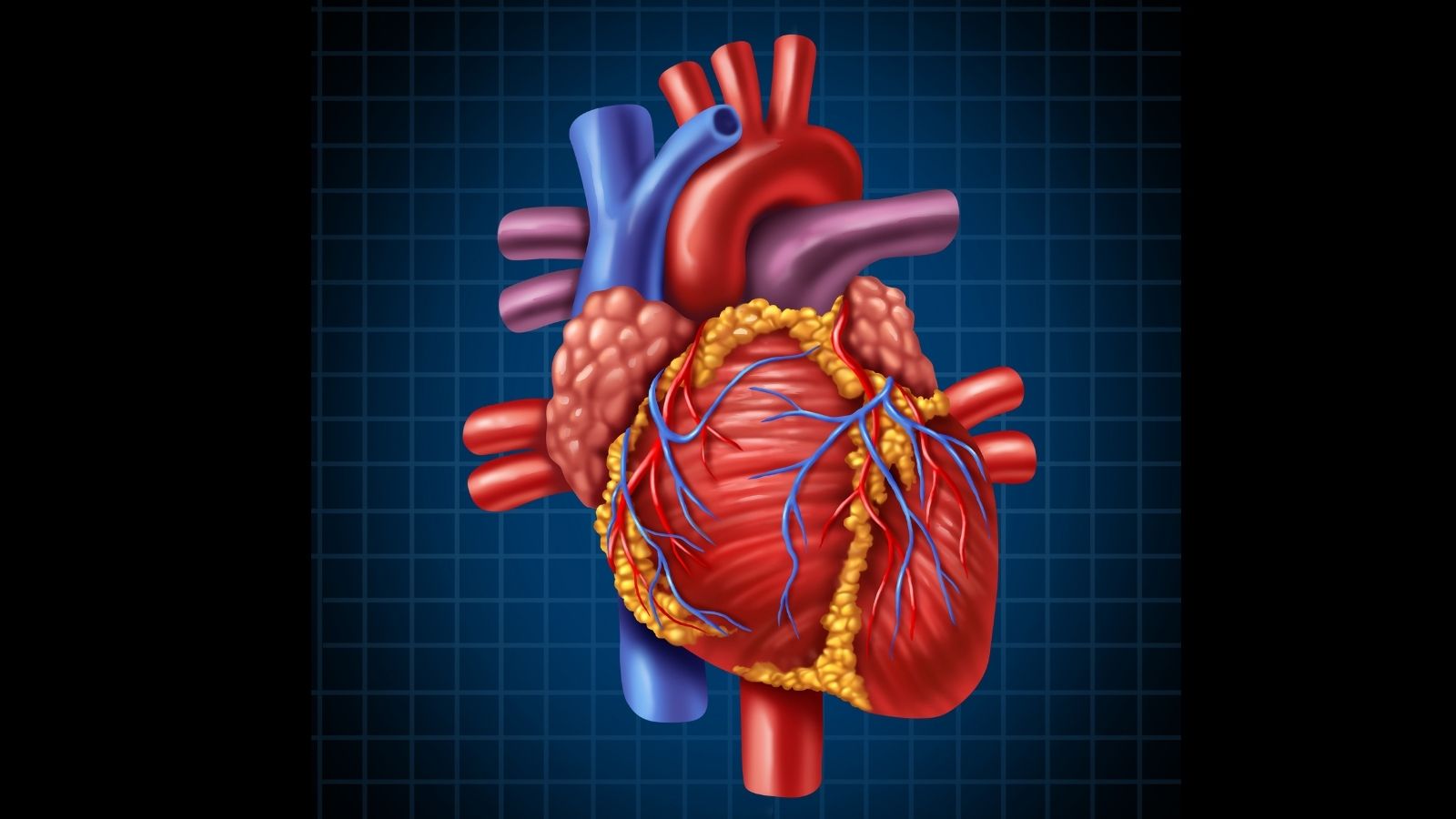
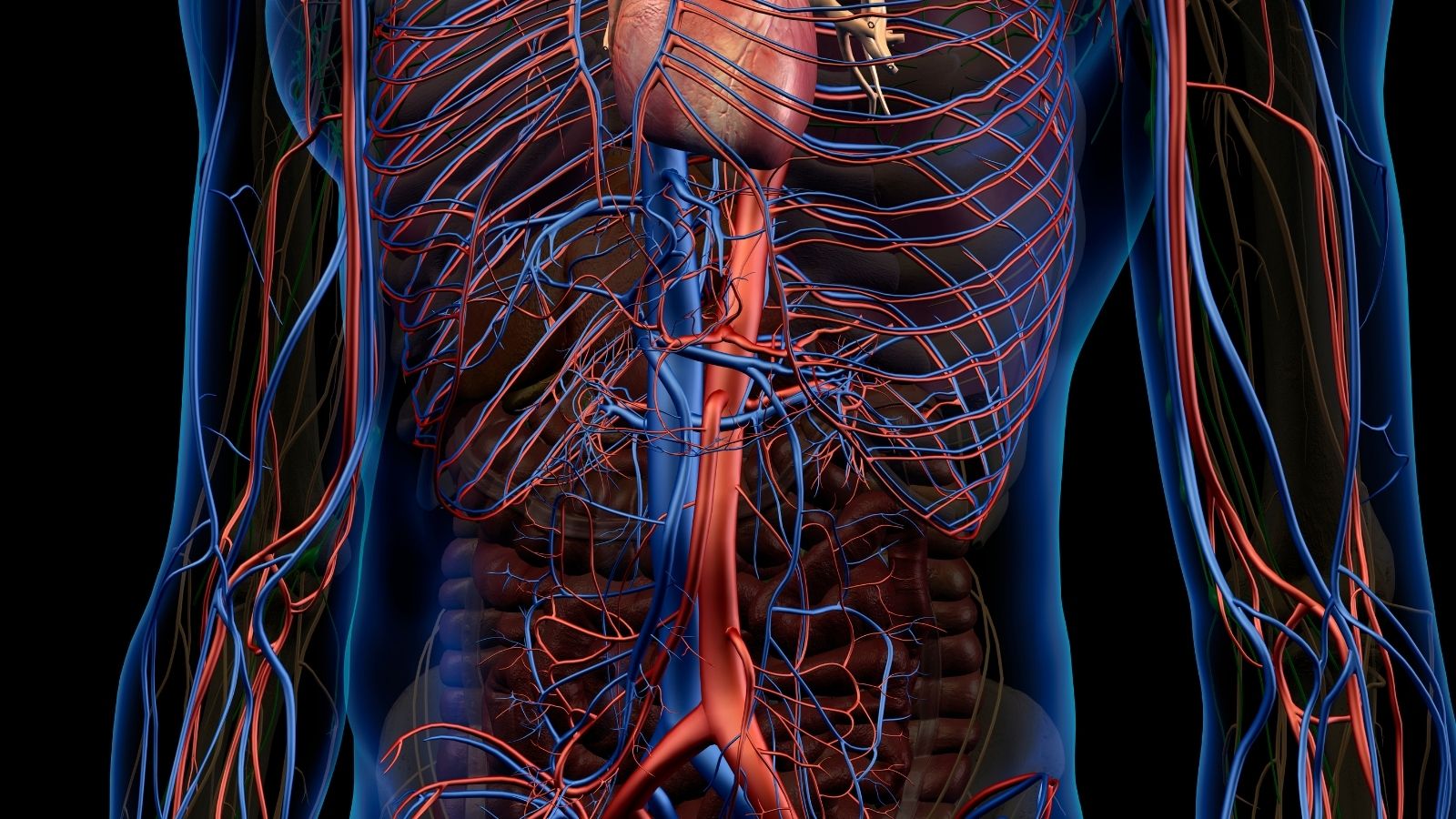
The aorta, the largest vessel in the body, can be compared to a layered garden hose that can withstand high pressure. This main pipeline, which carries blood pumped from the heart throughout the body, is made up of three sturdy layers. The innermost lining (intima) allows the blood to flow smoothly, in the middle is a muscular layer (media) that gives the vessel its flexibility and strength, and at the outermost is a protective sheath (adventitia).
A penetrating aortic ulcer (PAU) begins when a plaque that forms on the inner lining due to arteriosclerosis (atherosclerosis) cracks and erodes over time, forming a wound (ulcer) into the middle layer of the vessel. Under the influence of the blood pressure, this wound moves like a pocket or crater into the vessel wall.
PAU is actually a member of a group of conditions called “Acute Aortic Syndrome” (AAS), which requires urgent intervention. This group includes three dangerous conditions that develop suddenly in the aortic wall and have very similar symptoms. Differentiating between these conditions is vital for proper treatment.
The conditions that constitute Acute Aortic Syndrome are as follows:
- Acute Aortic Dissection (AAD): The most common type. A tear occurs in the inner lining of the aorta and blood enters through this tear, separating the layers of the vessel wall. This creates a second false pathway (false lumen) in the vessel through which blood flows.
- Intramural Hematoma (IMH): This is a leakage of blood into the middle layer of the vessel wall without an obvious tear in the inner lining of the vessel. It usually occurs as a result of rupture of very small capillaries (vasa vasorum) feeding the wall.
- Penetrating Aortic Ulcer (PAU): Deepening of the atherosclerotic plaque into the middle layer of the vessel. It is usually accompanied by intra-wall hemorrhage (hematoma).
These three conditions can actually be different faces of the same disease or stages that can trigger each other. For example, a small penetrating ulcer may eventually lead to an intra-wall hemorrhage (IMH), which may progress to a complete aortic dissection or rupture of the vessel. The diagnosis of PAU is therefore not only a snapshot but also an important sign of the overall wear and tear of the aortic wall and a warning of future risks.
How Does Penetrating Aortic Ulcer Occur and How Is It Related to Arteriosclerosis?
The underlying cause of a penetrating aortic ulcer is atherosclerosis, the silent progression of atherosclerosis over many years. This process can be likened to the buildup of rust and lime in an old water pipe over time. Over the years, under the influence of factors such as high cholesterol, smoking and high blood pressure, plaques consisting of fat, cholesterol and calcium build up on the aortic wall. These plaques harden and thicken the normally flexible vessel wall and, most importantly, weaken its structure.
The process of ulcer formation begins when the surface of one of these plaques cracks or erodes. Under the constant influence of high blood pressure, the damage to this weak spot deepens and penetrates the inner lining (intima) of the aorta, reaching the middle layer (media). This creates a cavity, a crater in the vessel wall.
From this point on, the blood pumped with each beat of the heart begins to leak through this weak spot into the vessel wall and can trigger a chain of events. The process could go like this:
- A local hemorrhage (intramural hematoma) starts inside the vessel wall.
- The bleeding expands and causes the vessel to balloon outwards (pseudoaneurysm or false aneurysm).
- The process can progress to a full-thickness dissection.
- In the worst case scenario, all layers of the vessel wall rupture (rupture) and fatal internal bleeding occurs.
Interestingly, arteriosclerosis plays a dual role here. On the one hand, it is the main culprit in initiating the disease, but on the other hand, a severely calcified vessel wall can sometimes act like an “armor” and limit the spread of bleeding. This is one of the factors that explains why ulcers progress slowly in some people and become dangerous very quickly in others.
Who is at Risk for Penetrating Aortic Ulcer?
Penetrating aortic ulcer is typically a disease of the elderly, as it is usually the result of many years of vascular wear and tear. While classical aortic dissection can occur at a younger age, PAU usually occurs in male patients in their 60s and 70s.
There are major risk factors that predispose to the development of this disease. These risk factors are:
- Advanced age
- Male gender
- Hypertension (high blood pressure)
- Cigarette smoking
- Hyperlipidemia (high cholesterol and triglyceride levels)
- Diffuse atherosclerosis (arteriosclerosis)
It is quite common for people diagnosed with PAU to also have diseases that affect other vessels in the body. This suggests that the problem is not limited to the aorta, but is a generalized vascular disease. Common accompanying conditions include the following:
- Coronary artery disease (blockage in the vessels feeding the heart)
- Chronic obstructive pulmonary disease (COPD)
- Peripheral arterial disease (especially blockage in the leg veins)
- Abdominal aortic aneurysm (Abdominal aortic aneurysm)
Very rarely, PAU can also occur in young people with genetic connective tissue diseases such as Marfan syndrome or as a result of infection of the vessel wall. In such cases, the underlying cause should be investigated separately.
What Symptoms Does a Penetrating Aortic Ulcer Cause in the Body?
The most typical symptom of a penetrating aortic ulcer is sudden onset and extremely severe chest or back pain. However, a significant proportion of patients may not feel any symptoms and the diagnosis may be made completely by chance.
In symptomatic patients, pain often has very characteristic features. These symptoms include:
- Sudden and very severe onset of pain
- pain character with a “tearing” or “stabbing” sensation
- Pain felt in the anterior chest wall or between the two shoulder blades
- Pain that can sometimes radiate to the neck, jaw or arms
Unlike a heart attack, this pain is most intense from the moment it starts and usually peaks within minutes.
On the other hand, the number of asymptomatic patients is not small. Today, many people who undergo computed tomography for other health problems (e.g. lung or abdominal scans) may be found to have a penetrating aortic ulcer by chance. While this can be a major concern at first, studies have shown that asymptomatic ulcers usually progress slowly and pose no immediate danger.
In rare cases, bleeding around the ulcer or an aneurysm can put pressure on neighboring organs and cause other symptoms. These rare symptoms include:
- Hoarseness (as a result of compression of the nerve to the vocal cords)
- Bloody sputum (as a result of ulcer opening into the respiratory tract)
- Fainting (due to sudden drop in blood pressure or severe pain)
Whether a patient is symptomatic or not is the most important factor determining how risky the disease is and the treatment plan.
How to Confirm the Diagnosis of Penetrating Aortic Ulcer?
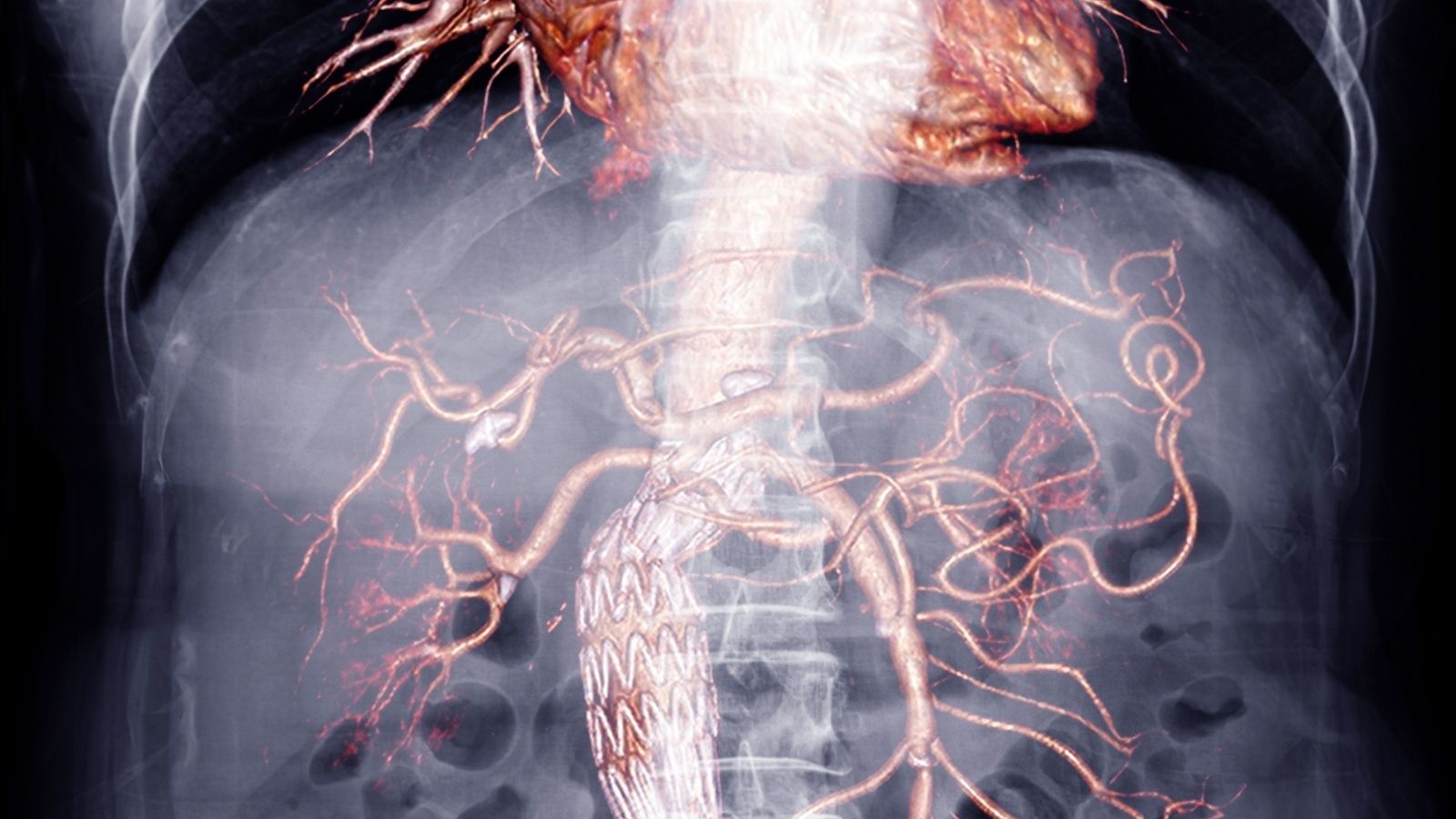
When a penetrating aortic ulcer is suspected, we use modern imaging modalities to confirm the diagnosis and understand the severity of the disease. The gold standard in this process is Computed Tomography Angiography (CTA), a medicated tomography method.
This special CT scan is performed by intravenously administering a dyed drug called a “contrast agent” and allows us to see the aortic vessel in three dimensions, down to the finest detail. With CTA, we not only confirm the presence of an ulcer, but also obtain invaluable information that will influence the treatment decision.
The findings we pay particular attention to in the CTA scan are the following:
- A pocket filled with contrast material extending outward from the aortic wall (ulcer crater)
- Depth and width of the ulcer
- The presence and thickness of an ulcer-related intra-wall hemorrhage (intramural hematoma)
- Total diameter of the aortic vessel at the site of the ulcer
These measurements help us to determine the risk of ulcer rupture and to decide which treatment method (medication, closed surgery or open surgery) is best for the patient.
There are other imaging methods that can be used in the diagnostic process. These methods are:
- Magnetic Resonance Imaging (MRI/MRA): This non-radiation method also shows the aorta in detail and may be more sensitive than tomography, especially in distinguishing whether the bleeding in the wall is new or old. However, it is not the first choice in emergencies due to the long acquisition time.
- Transesophageal Echocardiography (TEE): This examination, which is performed by inserting a thin ultrasound probe through the esophagus, shows the aorta in the rib cage very clearly. However, it may be insufficient to show some parts of the aorta (for example, the curve of the aorta).
- Chest X-ray: A standard X-ray is not diagnostic on its own. However, it may show indirect signs such as an enlargement of the aortic shadow and may raise suspicion.
What are the Dangerous Consequences of a Penetrating Aortic Ulcer?
The prognosis of a penetrating aortic ulcer varies greatly depending on the individual and the characteristics of the ulcer. An asymptomatic, small ulcer can remain stable for years, while a painful and large ulcer can lead to a fatal condition within hours.
There are major dangerous complications that can occur if the disease progresses. These complications include:
- Aortic Dissection: When an ulcer acts as a gateway for blood to seep between the layers of the vessel wall and tear it open.
- Aneurysm Formation: The weakened vessel wall balloons outward over time into a sac-shaped (saccular) or fusiform (fusiform) aneurysm.
- Aortic Rupture: The most feared complication. This is when the ulcer breaks through all layers of the vessel wall, causing a complete rupture, and the blood in the aorta empties into the chest or abdominal cavity. This is almost always fatal.
Some of the features we have found in imaging studies indicate a high risk of the ulcer progressing to these dangerous complications. These high-risk symptoms often require urgent treatment. Signs of high risk include:
- Ulcer depth of more than 10 mm
- Ulcer width of more than 20 mm
- Diameter of the affected aortic segment exceeds 45-50 mm
- The presence of a large and progressive intra-wall hemorrhage (hematoma) with the ulcer
- Pain that does not go away or recurs despite intensive medication
The presence of these risk factors requires a more active treatment plan rather than a “wait and see” approach, even in a patient without symptoms.
What are the Current Treatment Methods for Penetrating Aortic Ulcer?
The treatment of a penetrating aortic ulcer is planned with a “tailor-made” approach, i.e. completely individualized to the patient. Many factors such as the patient’s age, general health, the presence or absence of symptoms, the location of the ulcer in the aorta and risk characteristics are taken into consideration. Our main goal in treatment is to prevent fatal complications such as aortic rupture.
The most important distinction when determining the treatment plan is which part of the aorta the ulcer is in:
- Type A (Ascending Aorta): If the ulcer is in the first part that exits the heart, the condition is always considered high risk and emergency open-heart surgery is usually the only treatment option. This is because a tear in this area can cause blood to fill directly into the sac surrounding the heart (cardiac tamponade), leading to death within seconds.
- Type B (descending aorta): If the ulcer is in the descending part of the aorta towards the back and abdomen, the treatment approach is more variable. In uncomplicated patients, i.e. those without high-risk features and without symptoms, drug treatment and close follow-up are preferred.
According to this distinction, there are three main treatment modalities that we apply today:
- Medical (Drug) Treatment: Aims to reduce stress on the aortic wall by lowering blood pressure and heart rate.
- Endovascular Treatment (TEVAR): It is the closure of the ulcerated area with a stent-graft using a closed method through the inguinal vein.
- Open surgery: This involves opening the chest cage and removing the diseased aortic section and replacing it with an artificial vessel (graft).
When and How Is Drug Therapy Administered in the Treatment of Penetrating Aortic Ulcer?
Drug therapy is the first-line therapeutic approach, especially in patients in the descending part of the aorta (Type B), who are asymptomatic and do not have high-risk features (large diameter, deep ulcer, etc.). This is not a passive “waiting” process, but rather an active treatment strategy aimed at reducing stress on the aortic wall.
The main goals of drug treatment are:
- Blood Pressure Control: The goal is to aggressively lower blood pressure, usually to keep large blood pressure below 120 mmHg.
- Heart Rate Control: The goal is to slow the heart rate to reduce the impact of the blood hitting the vessel wall with each stroke.
- Cholesterol Management: By lowering cholesterol levels with statin group drugs, the progression of the underlying atherosclerosis is slowed down.
- Pain Control: In the initial stabilization of symptomatic patients, pain relief is important for both patient comfort and stress reduction.
Patients receiving medication are kept under very close clinical and imaging follow-up. At certain intervals (usually 6 months or 1 year), the status of the ulcer is checked with repeated CT scans. If, during this follow-up period, it is found that the ulcer has grown, the aneurysm has enlarged or the patient has started to experience pain, the treatment strategy is changed to interventional methods (TEVAR or open surgery).
What is Endovascular Treatment for Penetrating Aortic Ulcer (TEVAR)?
TEVAR stands for “Thoracic Endovascular Aortic Repair” and has become the standard treatment for complicated or high-risk penetrating aortic ulcers in the descending aorta (Type B). This is a closed procedure performed through a small incision in the groin artery without the need for major breast surgery.
The procedure is similar to lining a damaged pipe with a new pipe from the inside. During the procedure, a thin tube called a catheter is inserted through the groin vein and, under X-ray visualization, accesses the ulcerated area in the aorta. Through this catheter, a fabric-covered metal cage called a “stent-graft” is advanced. Once in the correct position, this stent-graft is opened and inserted into the vessel wall. The stent-graft completely closes the ulcer, cutting off the blood supply to the ulcer and creating a new, solid pathway for blood flow. This protects the weakened aortic wall from the stress of blood pressure.
TEVAR is a suitable option for patients who
- Those with severe pain that does not go away despite medication
- Those with high risk features detected on imaging even if asymptomatic (deep/wide ulcer, large aortic diameter, etc.)
- Those observed to have an enlarged ulcer or aneurysm during follow-up
- Developed aortic rupture or leakage due to ulcer
The main advantages of TEVAR over open surgery are that the risk of surgery is lower, blood loss is minimal and patients recover much faster and return to their normal lives. However, this procedure also has its own risks and patients should be followed up with regular tomography for life after the procedure.
When Is Open Surgery for Penetrating Aortic Ulcer Necessary?
Despite all the advances in endovascular therapy (TEVAR), open surgery is still the indispensable and gold standard treatment in certain situations.
In cases where open surgery is absolutely necessary, the ulcer is located in the part of the aorta (Type A) that exits the heart. This area always requires urgent open surgery due to its proximity to the heart and the severe consequences in case of rupture.
Other situations where open surgery is preferred are as follows:
- The ulcer is located in a complex area anatomically unsuitable for TEVAR, such as the aortic arch from which the brain and arm vessels arise
- Conditions such as Marfan syndrome, where the entire aortic tissue is genetically weak and a stent-graft cannot hold securely
- Patients who have failed a previous TEVAR procedure or developed stent-graft-related complications
- Patients who are young and in very good general health and can easily tolerate the risk of open surgery
In open surgery, the chest is opened and the patient is connected to a heart-lung machine. The surgeon completely removes the diseased aortic section containing the ulcer and replaces it with a synthetic, durable artificial vessel (graft) called a “Dakron”. Although this method is a larger operation, it may offer a more permanent solution in the long term as the diseased tissue is completely removed.
What Should Life Be Like After Penetrating Aortic Ulcer Treatment?
Treatment of a penetrating aortic ulcer, whether with medication, closed or open surgery, is not the end of a process but the beginning of a new way of life. The long-term success of treatment depends on how well the patient adapts to this new process.
There are the most important points to be considered in the post-treatment process. These points are:
- Regular medical check-ups and imaging: Regardless of the treatment, it is mandatory to check the aorta with computed tomography or MR angiography at regular intervals throughout life (more frequently in the first year, then annually).
- Blood Pressure Management: Keeping blood pressure under strict lifelong control is perhaps the most important rule. The goal is usually a large blood pressure below 120-130 mmHg.
- Cholesterol Control: Regular use of cholesterol medications is critical to maintain the health of both the repaired area and the rest of the aorta.
- Strict Smoking Cessation: Smoking is the number one enemy of vascular health. In order not to jeopardize the success of the treatment, smoking and all tobacco products should be avoided.
- Healthy Diet: A diet rich in vegetables, fruits and fiber and low in salt and saturated fats, such as the Mediterranean diet, should be adopted.
- Physical Activity: Aerobic exercises such as regular walking should be done as permitted by the doctor. However, strenuous movements such as lifting heavy weights that suddenly increase blood pressure should be avoided.
Frequently Asked Questions
What is a penetrating aortic ulcer?
It is a serious vascular disease that occurs when the atherosclerotic plaque on the inner surface of the aorta ulcerates and progresses to the middle layer of the vessel.
How dangerous is this situation?
It is very dangerous because it can lead to fatal complications such as aortic dissection or aortic rupture.
Who gets it?
It is most common in the elderly, hypertensive and arteriosclerotic individuals.
What is the difference between penetrating ulcer and aortic dissection?
A dissection is a tear along the vessel wall, whereas an ulcer is a limited and localized injury, but can develop into a dissection.
What are the symptoms?
Sudden onset of back or chest pain, shortness of breath, sweating and low blood pressure may occur.
How is it diagnosed?
It can be clearly visualized by CT angiography, MR angiography or transesophageal ECHO.
Why does a penetrating aortic ulcer occur?
It occurs when atherosclerotic plaques rupture over time and weaken the vessel wall.
Are there any cases that need follow-up?
Yes, small and stable ulcers can be monitored with regular follow-up and medical treatment.
Which cases need surgery?
Surgical intervention may be necessary if the ulcer is growing, dissection has started or the patient is experiencing severe symptoms.
Is endovascular treatment possible?
Yes, a stent graft can be applied with the TEVAR (thoracic endovascular aortic repair) method.
Is this disease fatal?
Without early diagnosis and appropriate treatment, the risk of death is high. Urgent intervention is required, especially if a rupture develops.
Is medication possible?
In mild cases, conservative treatment such as blood pressure control, cholesterol-lowering drugs and smoking cessation can be applied.
Which specialty is involved?
Cardiovascular surgery, interventional radiology and cardiology specialists work together.
Does penetrating aortic ulcer recur?
If risk factors are not controlled, it can recur with ulceration of new plaques.
What are the prevention methods?
It can be prevented with blood pressure control, cholesterol reduction, smoking cessation and regular check-ups.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.