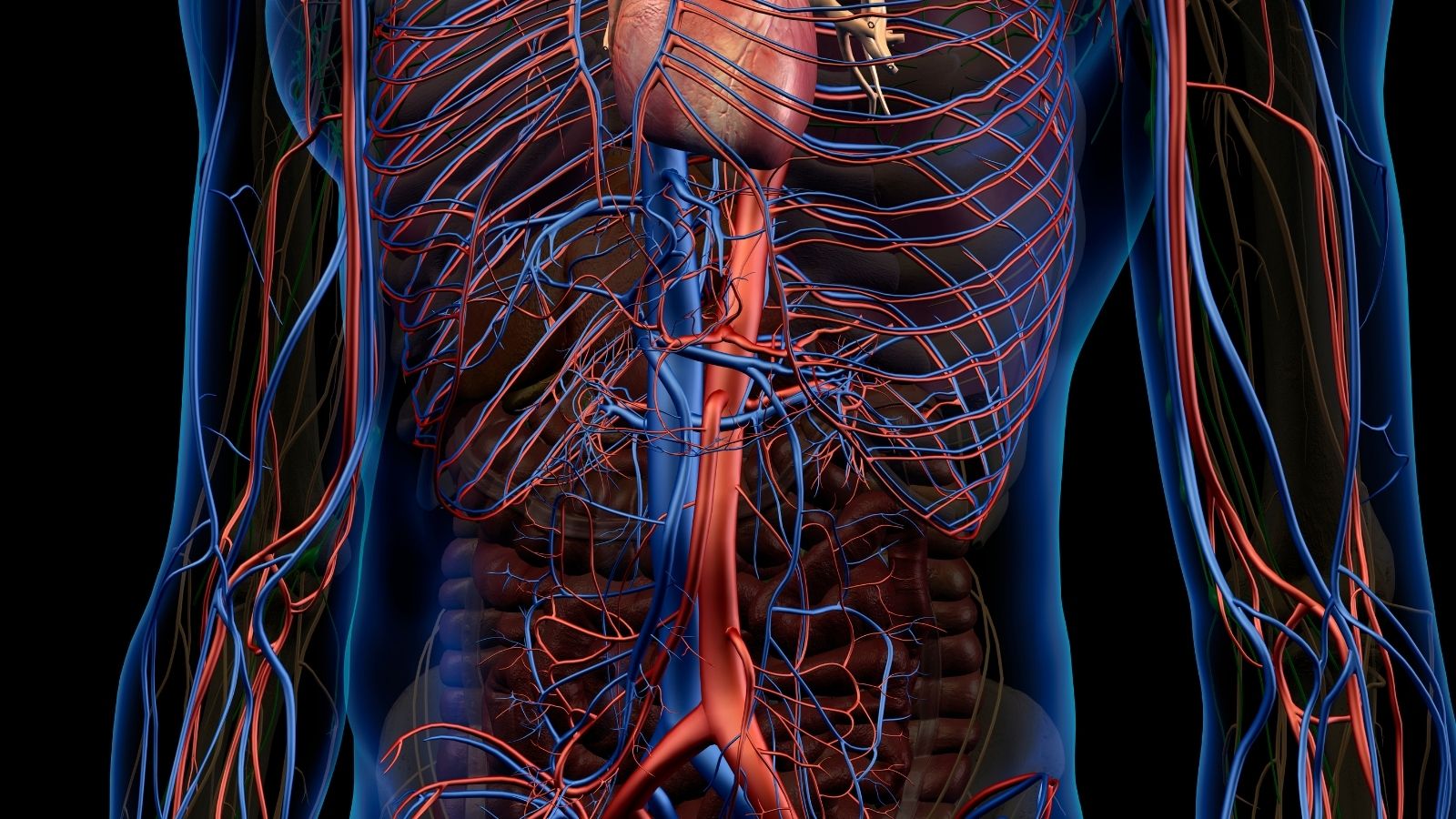
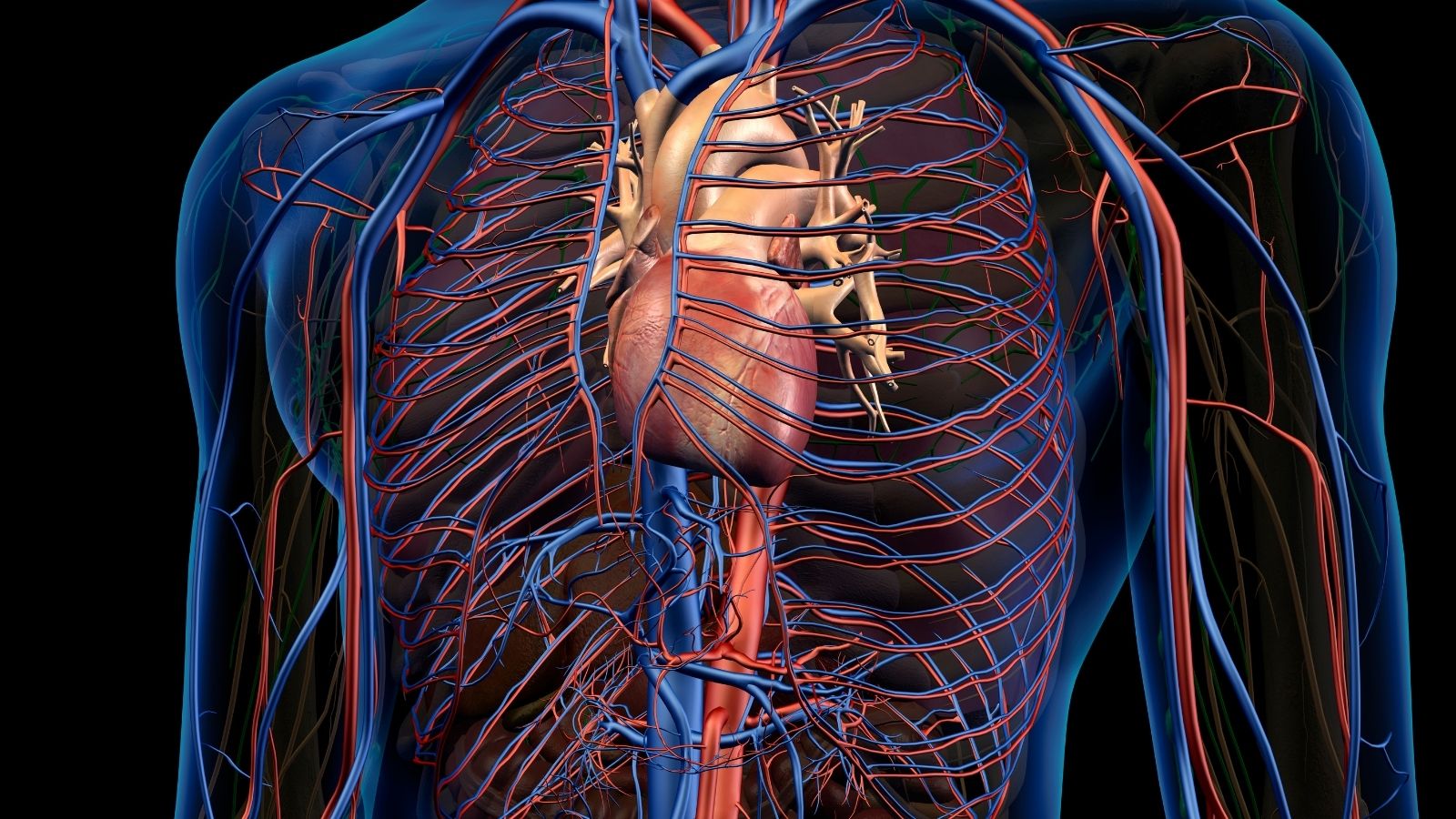
A thoracoabdominal aortic aneurysm is a serious enlargement of the aorta extending from the chest into the abdominal cavity. This condition carries a high risk of rupture and requires careful monitoring and timely surgical management.
The classification of thoracoabdominal aortic aneurysms is based on the extent of involvement of thoracic and abdominal segments. This anatomical detail is crucial, as it determines surgical strategy and potential complications affecting visceral arteries.
Risk factors for thoracoabdominal aortic aneurysm include hypertension, atherosclerosis, connective tissue disorders, and genetic predisposition. Smoking and advanced age further increase the likelihood of aneurysm development and progression.
Treatment typically involves open surgical repair or endovascular stent grafting, depending on patient condition and aneurysm morphology. Preoperative planning and postoperative monitoring are essential to reduce morbidity and improve survival rates.
| Definition | Abnormal aortic dilatation involving both thoracic (chest) and abdominal (abdomen) aortic segments |
| Classification | Evaluated by Crawford classification (Type I-IV); classified according to the extent of the aneurysm in the thoracic and abdominal aorta |
| Causing Factors | Atherosclerosis, Marfan and Ehlers-Danlos syndromes, chronic dissection, vasculitis (e.g. Takayasu, Behçet’s), trauma |
| Risk Factors | Hypertension, smoking, dyslipidemia, connective tissue diseases, family history |
| Symptoms | May be asymptomatic; back, abdominal or chest pain, weight loss, weakness, compression symptoms |
| Diagnostic Methods | CT angiography (gold standard), MRI, thoracoabdominal aortic angiography, physical examination findings are often insufficient |
| Complications | Rupture, spinal ischemia (paraplegia), visceral ischemia, renal failure, thromboembolism |
| Treatment Methods | Open surgical repair (replacement with graft), endovascular approach (TEVAR EVAR combination), hybrid surgical methods |
| Follow-up and Monitoring | Monitoring diameter and morphology with regular imaging, blood pressure control, early detection of complication development |
| Ways of Prevention | Control of risk factors (hypertension, smoking, lipid levels), monitoring of genetic syndromes, regular screening (especially if there is a family history) |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
Why is Thoracoabdominal Aortic Aneurysm a Major Health Problem?
Thoracoabdominal aortic aneurysm, although rare, is a condition that should be taken extremely seriously when diagnosed. This is mainly because of the silent but devastating risks it carries. Thanks to the aging population and advanced imaging methods such as Computed Tomography (CT), these aneurysms are now being diagnosed more frequently.
The greatest danger is that the wall of the aneurysm can no longer hold on and ruptures, i.e. ruptures. This is a catastrophe that leads to massive internal bleeding inside the body that is very difficult to stop and is almost always fatal without immediate intervention. It is known that most of these untreated aneurysms eventually rupture and the chances of long-term survival for these patients are very low.
The most important factor determining the risk is the size of the aneurysm; the larger the diameter, the greater the risk of rupture. Surgical intervention is usually recommended when the aneurysm diameter reaches 5.5 to 6.0 cm, as the risk of rupture increases to unacceptable levels.
There are other dangers besides rupture. Blood clots that form in the aneurysm can break off and travel through the bloodstream to the brain, causing a stroke or block leg veins, leading to gangrene. It can also cause another type of tear in the vessel wall called “aortic dissection”, which in itself is a fatal emergency.
Perhaps the most frightening aspect of TAAA is that it usually gives no symptoms. This is why it is called the “silent killer”. Most devastating events occur without any warning signs. It is therefore fortunate for the patient if it is found by chance during an examination for another reason. Just because the patient feels well does not mean that there is no danger. It is not the patient’s complaints that determine the risk, but concrete measurements such as the size of the aneurysm. Understanding this fact explains why a physician might recommend major surgery on a person who feels perfectly healthy.
What Causes the Development of a Thoracoabdominal Aortic Aneurysm?
Understanding the reasons behind the development of thoracoabdominal aortic aneurysm and who is at greater risk is critical for both prevention and management. Risk factors can be categorized into two main groups: Degenerative process due to the wear and tear of the vasculature over the years and genetic process due to congenital structural weaknesses.
The leading cause is atherosclerosis, also known as hardening of the arteries. In this process, fat and lime plaques build up on the vessel wall, causing it to lose its elasticity and strength. Some important factors that accelerate atherosclerosis and increase the risk of aneurysms include
- Cigarette smoking
- High blood pressure (Hypertension)
- Advanced age
- Family history
- Male gender
Smoking is the strongest known risk factor; its chemicals directly damage the vessel wall. High blood pressure mechanically fatigues and weakens the aortic wall through constant pressure. The risk increases with age and is usually seen in people over the age of 65. A family history of aneurysm, especially in first-degree relatives, increases the risk several times. Although more common in men, an aneurysm in women is more likely to rupture at a smaller size.
The second group are genetic diseases that affect the body’s connective tissue. Connective tissue is a kind of “glue” that ensures the structural integrity of our body. A genetic defect in this tissue makes the aortic wall congenitally weak. There are several syndromes that lead to this condition:
- Marfan Syndrome
- Loeys-Dietz Syndrome (LDS)
- Ehlers-Danlos Syndrome (EDS), especially the vascular type
In people with these genetic syndromes, aneurysms may occur at a much younger age and follow a more aggressive course. Therefore, taking a detailed personal and family history of the patient plays a key role in determining the right treatment strategy. If there is a genetic predisposition, surgery may be recommended for smaller aneurysm sizes and different techniques may be used during surgery.
How Does an Enlarging Thoracoabdominal Aortic Aneurysm Present Itself?
Most thoracoabdominal aortic aneurysms, especially in the early stages, grow insidiously and cause no symptoms. For this reason, patients can often live unaware of the condition for years. However, as the aneurysm enlarges, it may start to put pressure on the surrounding tissues and organs, causing some vague symptoms. It is very important to distinguish these symptoms from signs of urgent rupture.
Possible symptoms of a stable aneurysm that is growing but has not yet ruptured are
- A deep, dull pain felt in the back, chest or abdomen
- Throbbing or pulsating sensation in the abdomen, like a heartbeat
- Shortness of breath or cough
- Difficulty swallowing
- Hoarseness
- Weakness or numbness in the legs
These symptoms can be caused by the aneurysm growing and pressing on the lungs, the esophagus, the nerve to the vocal cords or the spinal cord.
However, when the aneurysm wall ruptures (rupture) or the wall layers separate (dissection), the symptoms are much more sudden, severe and dramatic. This is an absolute medical emergency and requires a call to 112 without losing a second. Life-threatening symptoms at the time of rupture are as follows:
- Extraordinarily severe pain in the back, chest or abdomen, starting suddenly and described as “tearing”
- Sudden and severe dizziness or fainting
- Sharp drop in blood pressure
- Cold, sticky and pale skin
- Fast pulse
- Nausea and vomiting
- Intense anxiety and a feeling that something bad is going to happen
Knowing the difference between these two conditions can save lives. If you have vague but persistent back pain or a pulsating sensation in the abdomen, you should make an appointment to see a specialist. However, if a sudden and searing pain is accompanied by a feeling of fainting, this is a harbinger of disaster and emergency help should be called immediately.
How is Thoracoabdominal Aortic Aneurysm Diagnosed and Classified?
The definitive diagnosis of a thoracoabdominal aortic aneurysm is made thanks to modern technology that can image the inside of the body in detail. Although the process begins with listening to the patient’s complaints and medical history, imaging tests are essential for a final diagnosis. These tests not only confirm the presence of the aneurysm, but also reveal its size, exact location and all the anatomical details necessary for surgical planning.
The main imaging methods used in diagnosis are as follows:
- Computed Tomography (CT) Angiography
- Magnetic Resonance (MR) Angiography
- Echocardiography (especially TEE)
- Abdominal Ultrasound
The gold standard among these is CT angiography. This test creates a three-dimensional map of the aorta by injecting a special dye (contrast dye) into the vessel. MRI angiography does not involve radiation and is a good alternative, especially in younger patients or in cases where frequent follow-up is required. Ultrasound and echocardiography are mainly used for screening and initial evaluation.
It is vital that people at risk are screened, even if they do not have any complaints. Especially men over the age of 65 with a history of smoking and those with a family history of aneurysms should be evaluated by a specialist.
Once the aneurysm is diagnosed, one of the most important steps in surgical planning is classification. The Crawford Classification System, developed by Dr. Crawford and still widely used today, defines how much area the aneurysm covers on the aorta. This classification is like a road map for the surgeon and directly affects the complexity and risks of the surgery and the technique to be used.
- Type I: The aneurysm involves most of the chest aorta and the abdominal aorta above the kidney vessels.
- Type II: The largest and most challenging type. The aneurysm covers almost all of the chest aorta from the beginning to the end of the abdominal aorta. This type has the highest risk of stroke.
- Type III: The aneurysm starts in the lower parts of the chest and spreads into the abdomen.
- Type IV: The aneurysm is limited to the part of the aorta in the abdominal cavity.
- Type V: The aneurysm affects the area from the lower part of the rib cage to just above the kidney veins.
The higher this classification number (especially Type II), the more vital organ vessels the surgery involves, increasing the difficulty and risk of the operation.
Is Surgery Necessary for Every Thoracoabdominal Aortic Aneurysm?
No, not every patient diagnosed with a thoracoabdominal aortic aneurysm needs to go to the operating table immediately. If the aneurysm is small (usually less than 5.5 cm) and does not cause any symptoms, the dangers of a major and risky operation may be greater than the risk of the aneurysm rupturing at the time. The procedure in such cases is called “watchful waiting” or “active surveillance”.
But this does not mean ignoring the situation and waiting passively. On the contrary, it is a multifaceted management strategy in which the patient is actively involved in the treatment process. This strategy consists of three key components.
Surveillance with Regular Monitoring: This is the cornerstone of the process. The aim is to closely monitor the size and growth rate of the aneurysm. The diameter of the aneurysm is usually measured every 6 to 12 months with an imaging test such as CT or MRI. If the aneurysm reaches a dangerous size or grows faster than expected (e.g. more than 0.5 cm per year), then it is time for surgery.
Medical treatment: The aim of drug therapy is to slow the growth of the aneurysm by reducing the stress on the aortic wall. The aim is to keep blood pressure under very tight control. Blood pressure medications, such as beta-blockers and ARBs, not only lower blood pressure but also reduce the contractile force of the heart, relieving the stress on the aortic wall. In addition, statin cholesterol medications are usually added to the treatment to slow down atherosclerosis.
Lifestyle Changes: The biggest task in this regard falls to the patient. Healthy lifestyle habits to be adopted by the patient are critical for controlling risk factors and slowing down the process. The most important lifestyle changes to make are the following:
- Definitely quit smoking
- Avoiding heavy lifting
- Avoiding movements that require intense straining
- Learning to manage stress
- Adopting a heart-friendly diet low in salt and saturated fat
This process of careful waiting makes the patient the captain of their own health and allows for surgical intervention in the safest conditions when the time is right.
How is Thoracoabdominal Aortic Aneurysm Surgery Performed with Traditional Method?
For many years, the “gold standard” for the treatment of thoracoabdominal aortic aneurysm has been the traditional open surgical repair. This is one of the largest and most complex operations in cardiovascular surgery. The basic principle of the operation is to completely remove the diseased and ballooned aortic section and replace it with an artificial vessel (graft) made of a durable synthetic material such as Dacron.
This operation is performed through a large incision (thoracoabdominal incision) that extends from the left chest wall into the abdomen. This incision allows the surgeon to control the entire area where the aneurysm is located. During surgery, surgical clamps are placed above and below the aneurysm to stop the blood flow.
The most critical and challenging part of the operation is to protect the vital organs that remain anemic while the aorta is clamped. The spinal cord, kidneys and intestines are particularly vulnerable to this period of anemia. Surgeons use a number of advanced techniques to protect these organs from damage. These protective measures include:
- Left heart bypass
- Cerebrospinal fluid (CSF) drainage
- Lowering body temperature (hypothermia)
- Administration of cold protective solutions to the kidneys
With a left heart bypass, a machine pumps blood from the upper part of the body to the lower part, so that the organs can continue to receive blood. Drainage of cerebrospinal fluid through a catheter inserted in the back reduces the pressure in the spinal cord, reducing the risk of stroke. Under these protective measures, the surgeon removes the segment of the aorta with the aneurysm and sews an artificial vessel in its place. The vessels that supply vital organs such as the kidneys and intestines are reconnected to this new artificial vessel.
Although open surgery requires a long and difficult recovery period, it offers the most durable and long-lasting solution, especially for young patients in good general health. The success of this surgery depends not only on the experience of the surgeon but also on the technological equipment and multidisciplinary teamwork of the center where the surgery is performed.
Is Thoracoabdominal Aortic Aneurysm Treatment Possible with Modern Methods?
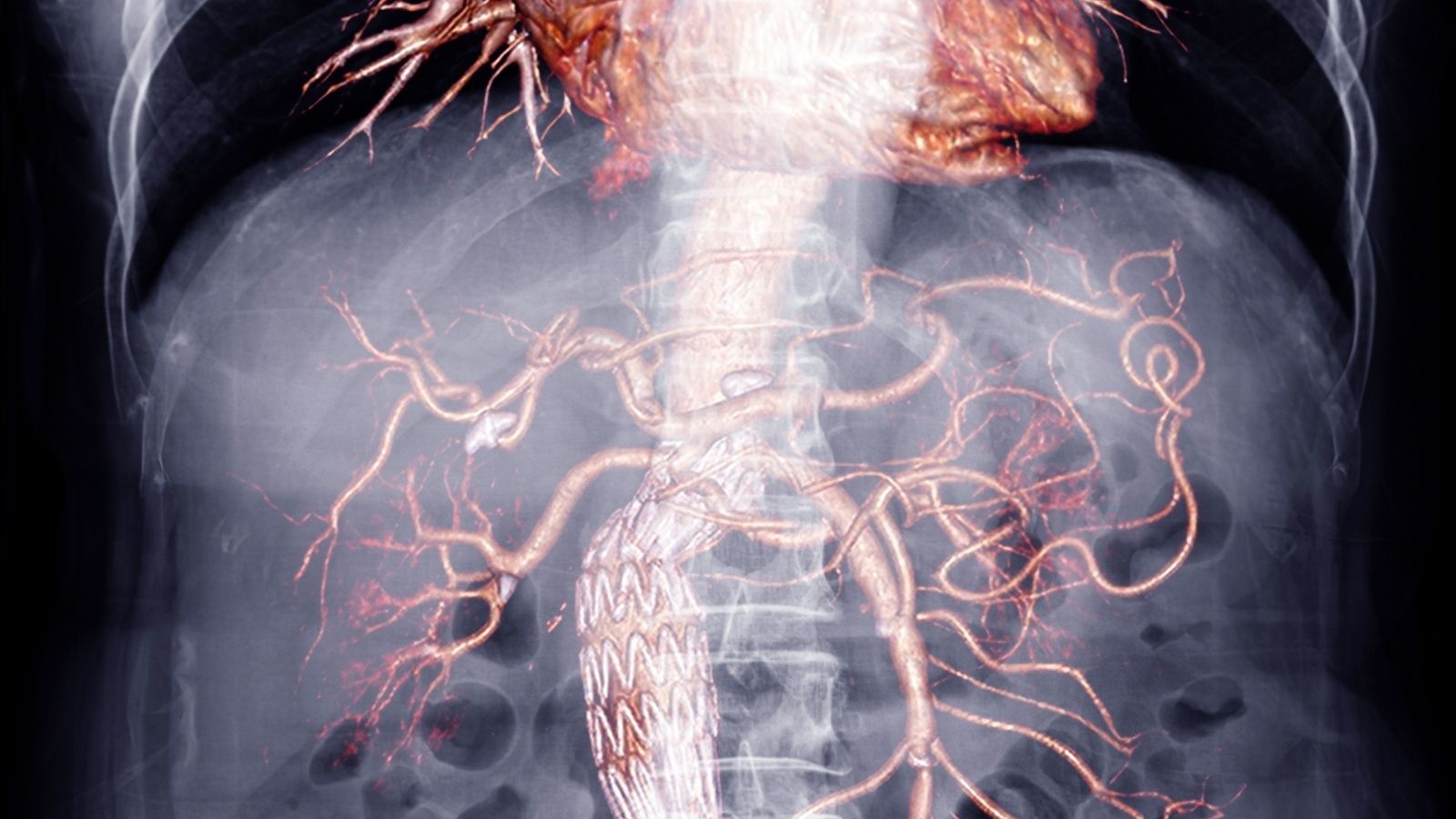
Yes, today thoracoabdominal aortic aneurysms can be treated with a modern and much less invasive method called “endovascular repair”. In this technique, instead of making a giant incision in the chest and abdomen, the entire procedure is performed under the guidance of an angiography device through small punctures in the arteries in the groin. This method is called FEVAR (Fenestrated EVAR) or BEVAR (Branched EVAR) depending on the structure of the special stent-graft used.
The basic principle of the operation is to move a folded stent-graft (a fabric-covered tube supported by a metal framework) through the vessels using catheters to the site of the aneurysm and open it there. This stent-graft attaches to the intact aortic wall above and below the aneurysm and creates a new blood pathway. The blood flows through this new tunnel without ever entering the aneurysm sac. The aneurysm sac, relieved of pressure, coagulates and shrinks over time, becoming harmless.
The most challenging part of this treatment is to preserve the blood flow to the kidney and intestinal vessels exiting the aneurysm site. FEVAR and BEVAR technologies have been developed to solve this problem. In the FEVAR technique, the stent-graft has small windows (fenestrations) pre-planned to coincide with the mouths of these vessels. In the BEVAR technique, there are small side branches (branches) emerging from the body of the stent-graft. Through these windows or branches, blood flow to the organs is maintained.
Endovascular repair has some important advantages over open surgery:
- Less invasive
- Lower risk of surgery
- Very little blood loss
- The healing process is much faster
- Shorter hospital stay
For these reasons, endovascular repair is an excellent alternative, especially for older patients or those with additional health problems for whom open surgery carries a high risk. However, this method may not be suitable for every patient. The patient’s vascular anatomy must be suitable for the safe placement of a stent-graft. It also comes at a price: a lifetime of close follow-up with regular CT scans and the possibility of needing additional minor interventions over time.
What is Hybrid Method in Thoracoabdominal Aortic Aneurysm Treatment?
Hybrid procedures are a personalized treatment strategy that combines the best aspects of open surgery and endovascular repair techniques for the treatment of thoracoabdominal aortic aneurysm. This approach is often considered a solution for anatomically challenging or very high-risk patients for whom standard open or endovascular treatment alone is not appropriate. As the name suggests, it is a hybrid treatment that combines elements of both open surgery and the closed (endovascular) method.
The most common hybrid technique is “visceral branching” followed by endovascular repair. In this method, the surgeon reroutes the blood flow to vital organs such as the kidneys, liver and intestines through a more limited open surgery, usually only in the abdomen. This is done by connecting new artificial vessels (bypass) from another healthy artery in the body to these organ vessels. Once this first step has been completed, the second step involves inserting a standard endovascular stent-graft through the groin to close the entire aneurysm sac. Since the blood supply to the organs is now secured by the new bypass vessels, this stent-graft can be safely implanted.
This approach avoids the huge chest incision and associated risks of a full open repair. Hybrid procedures are usually reserved for a very specific group of patients:
- Very elderly patients
- Those with severe heart or lung disease
- Those who are too weak to tolerate a full open surgery
- Those whose vascular anatomy does not allow standard endovascular repair (F/BEVAR)
- Patients for whom the standard approach would be too dangerous due to previous surgeries
Although hybrid procedures avoid opening the rib cage, they are still large and serious operations and carry their own risks. In particular, the long-term patency (non-obstruction) of the bypass vessels is important and requires close follow-up. Today, with the rapid development of full endovascular techniques such as FEVAR/BEVAR, the area of use of hybrid procedures has narrowed. Rather than being a routine treatment option, it is now seen as an important problem-solving tool at the surgeon’s disposal for the most challenging and selected cases where no other method is appropriate.
What are the Risks of Thoracoabdominal Aortic Aneurysm Surgery?
Thoracoabdominal aortic aneurysm repair is one of the most challenging and risky procedures in modern medicine, regardless of the method used. When deciding on this surgery, the serious risks of the operation are always weighed against the almost certain fatal outcome of the aneurysm rupture if left untreated. It should not be forgotten that when these operations are performed in high-volume and experienced centers, the chances of success are much higher than if the aneurysm is left alone.
The most important and feared risks of surgery are the following:
- Death during or immediately after surgery (Mortality)
- Paralysis of the legs due to spinal cord damage (Paraplegia)
- Renal failure and the need for dialysis
- Stroke (cerebral palsy)
- Heart attack
- Respiratory failure and pneumonia
- Disruption of intestinal blood supply (intestinal ischemia)
The risk of death depends on the experience of the center where the surgery is performed, the urgency of the operation and the general health status of the patient. While this rate is between 5-9% for open surgery in high-volume specialist centers, it falls below 3% for the endovascular (closed) method.
The risk of paralysis is considered the “Achilles heel” of this surgery and is the most feared complication. It results from the temporary interruption of blood flow to the spinal cord during surgery. In extensive open surgery, this risk can be as high as , whereas with the endovascular method it is usually lower. This risk is minimized by modern preventive measures during surgery.
Kidney failure is also an important risk. Temporary or permanent dialysis may be needed after surgery. This risk is also lower with the endovascular method compared to open surgery.
Despite these serious risks, it is important to remember that the main purpose of surgery is to prevent a certain catastrophe such as an aneurysm rupture. An operation performed by an experienced team, at the right time and with the right technique offers the patient the chance of a long and healthy life.
After Thoracoabdominal Aortic Aneurysm Surgery
| Recovery Time | Average 2-4 weeks; may vary depending on the patient’s age, general health status and the extent of the surgery. |
| Physical Activity | Light walking is recommended in the first weeks; a gradual return to daily activities is possible within 6-8 weeks. |
| Medication Use | Antihypertensive drugs, blood thinners and other prescription medications should be used regularly. |
| Nutrition | A low-sodium, low-fat, vegetable and fruit-based diet is recommended; cholesterol and blood sugar control is important. |
| Blood Pressure and Cholesterol Control | Blood pressure and cholesterol levels should be monitored regularly; target values should be set by the doctor. |
| Wound Care | Surgical incision sites should be kept clean and dry; signs of infection (redness, discharge, fever) should be monitored. |
| Infection Prevention | Especially if a prosthetic graft is used, the risk of infection is high; hygiene rules should be observed. |
| Sexual Activity | Depending on physical capacity, it can usually be started after 4-6 weeks, with the doctor’s approval. |
| Psychological Support | Anxiety and depression may occur; psychological support should be sought if necessary. |
| Controls | Cardiology and vascular surgery checks are recommended frequently in the first month and 1 or 2 times a year thereafter. |
| Smoking and Alcohol | Strongly not recommended; poses a serious risk to vascular health. |
| Vehicle Use | It can usually be started after 4-6 weeks, provided that reflexes and attention are appropriate. |

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.