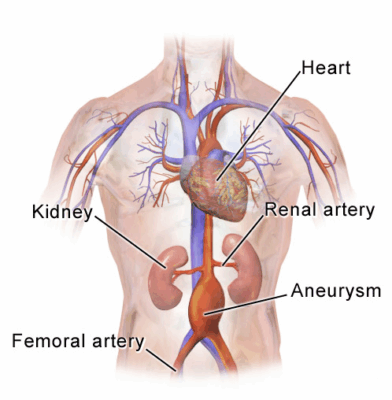
An abdominal aortic aneurysm is a pathological dilation of the abdominal aorta, often caused by arterial wall weakening. This condition is life-threatening if rupture occurs, making early diagnosis and monitoring essential. Symptoms may be absent until advanced stages.
Risk factors for abdominal aortic aneurysm include hypertension, smoking, advanced age, and family history. Screening programs, particularly with ultrasound, are recommended for high-risk groups to ensure early detection before rupture risk increases.
Treatment options for abdominal aortic aneurysm vary depending on aneurysm size and growth rate. While small aneurysms may be monitored, larger or rapidly enlarging aneurysms often require surgical intervention through open surgery or endovascular repair.
Post-treatment management involves strict cardiovascular monitoring, blood pressure control, and lifestyle adjustments. Long-term follow-up ensures prevention of recurrence or complications, supporting patient safety and improving survival outcomes.

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
| Medical Name | Abdominal Aortic Aneurysm (AAA) |
| Type | Aneurysmatic vessel disease |
| Affected System | Cardiovascular system (abdominal aorta) |
| Causes | Atherosclerosis (most common), hypertension, smoking, advanced age, male gender, genetic predisposition |
| Symptoms | Usually asymptomatic; sudden abdominal/back pain, hypotension, loss of consciousness |
| Diagnostic Methods | Abdominal ultrasonography (screening), CT angiography (detailed imaging), MR angiography |
| Treatment Methods | Follow-up for small aneurysms; surgical intervention for those >5.5 cm or symptomatic: open surgery or endovascular aneurysm repair (EVAR) |
| Complications | Rupture (high mortality), thrombosis, distal embolization, organ ischemia |
| Observation | Monitoring every 6-12 months depending on aneurysm size, control of risk factors (smoking cessation, hypertension treatment), postoperative follow-up (control of graft patency after EVAR) |
Why and How Does an Abdominal Aortic Aneurysm Occur?
The wall of our aorta is made up of special protein fibers (elastin and collagen) that provide strength and flexibility against pressure, just like the supporting layers inside a tire. An aneurysm begins when the structure of these fibers breaks down. The most common and most important culprit behind this deterioration is “atherosclerosis”, or arteriosclerosis as we all know it.
Arteriosclerosis is the accumulation of fat, cholesterol and some other substances over the years in the vessel walls, forming structures we call “plaques”. These plaques initiate a chronic, low-level inflammation of the vessel wall. This inflammatory environment activates enzymes that gradually break down the precious protein fibers that keep the vessel wall intact. Over time, the vessel wall weakens, becomes thinner and loses its elasticity. Under the constant pressure of blood pressure from every beat of the heart, this weak spot begins to expand outward, like a balloon in an old car tire. An aneurysm is diagnosed when the diameter of the abdominal aorta exceeds 3 cm, compared to about 2 cm in a healthy person. When this enlargement reaches a critical threshold of 5.5 cm, treatment becomes necessary as the risk of rupture increases significantly.
Who is at Risk for Abdominal Aortic Aneurysm?
Some factors are more prominent in the development of aneurysms. These factors can be divided into two groups: those that we can change and those that we cannot. These lists will guide you as you assess your own situation.
Risk factors that cannot be changed, i.e. that are beyond our control, are the following:
- Age (especially over 65 years)
- Male gender
- Family history of aneurysm
- Some genetic connective tissue diseases (Marfan, Ehlers-Danlos)
- White race
The risk factors that we can change, that is, that we can directly influence through our lifestyle choices, are as follows:
- Smoking
- High blood pressure (Hypertension)
- High cholesterol (Hyperlipidemia)
- Arteriosclerosis present in other vessels of the body
Among these lists, one factor stands out more than any other: Smoking. Smoking is the largest and most important single risk factor for aneurysm development. The thousands of harmful chemicals in cigarette smoke directly damage the valuable structural proteins in the vessel wall and accelerate the process of atherosclerosis to an incredible degree. This is why a smoker’s risk of developing an aneurysm is many times higher than someone who has never smoked. Family history is also very important. If your mother, father or brother or sister has been diagnosed with an abdominal aortic aneurysm, your susceptibility to the condition is increased and you need to be more careful. The occurrence of aortic aneurysms at a young age is often associated with these genetic predispositions.
How to Reduce the Risk of Developing an Abdominal Aortic Aneurysm?
Reducing the risk of an aneurysm or slowing the growth of an existing small aneurysm is basically a matter of protecting our vascular health as a whole. This is not only a recommendation, but also the cure for small aneurysms. The most effective steps you can take are the following:
- Definitely quit smoking
- Keeping blood pressure at ideal levels
- Controlling cholesterol levels
- Reducing salt consumption
- Eating a healthy and balanced diet
- Regular physical activity
- Maintaining ideal weight
- Learning to manage stress
These lifestyle changes will not eliminate or reduce an aneurysm. So why are they so important? Because these steps put the brakes on the underlying problems that cause an aneurysm to form and grow – atherosclerosis and inflammation in the vessel wall. It’s like stopping throwing wood on a burning fire; even if the fire doesn’t go out immediately, it is prevented from growing further. In particular, keeping blood pressure under control plays a vital role in slowing the rate of growth, as it reduces the constant stress on the aneurysm wall. Regular use of blood pressure and cholesterol medications (such as statins) prescribed by your doctor for this purpose is the most important part of this process.
What are the Symptoms of a Growing Abdominal Aortic Aneurysm?
The most worrying aspect of an abdominal aortic aneurysm is that it often causes no symptoms as it grows for years. This is why it is called the “silent killer”. A significant proportion of diagnoses are made completely incidentally during an ultrasound or CT scan in patients who see a doctor with another complaint (e.g. gallbladder or kidney stone).
However, as the aneurysm grows and begins to put pressure on surrounding tissues, some vague symptoms may occur. Symptoms of an abdominal aortic aneurysm include the following:
- A persistent, deep, gnawing pain felt in the abdomen, back or side
- A pulsation or throbbing around the navel, especially when lying on the back, synchronized with the heartbeat
- Feeling of early satiety or fullness even with very little food
These symptoms are not always visible and usually occur after the aneurysm has reached a certain size. A palpable, pulsating mass in the abdomen is a very typical finding, especially in people of thin build.
What are the Symptoms of a Ruptured Abdominal Aortic Aneurysm?
Aneurysm rupture (rupture) is the most urgent and life-threatening condition in vascular surgery. This means that the wall of the aneurysm can no longer withstand the blood pressure and ruptures, allowing blood to drain rapidly into the abdominal cavity. Recognizing this picture and seeking medical help without losing a second saves lives.
The alarming symptoms of a ruptured aneurysm are the following:
- Sudden onset of unusually severe abdominal or back pain of a tearing or stabbing nature
- Dangerous drop in blood pressure
- The heart beats too fast to compensate
- Severe dizziness or fainting
- Skin becomes cold, pale and sweaty
- Shortness of breath
- Nausea and vomiting
These symptoms are signs of massive internal bleeding and the body going into shock. The only thing to do in such a situation is to call the 112 emergency hotline immediately. The sooner the hospital is reached and the sooner surgery is performed, the better the chances of survival. Unfortunately, a significant proportion of patients with ruptured aneurysms die before reaching the hospital. This painful fact makes it clear why aneurysms should be detected and treated in the “silent” phase, before they rupture.
What Are Other Complications of an Untreated Abdominal Aortic Aneurysm?
Although rupture is the most feared outcome, there are other dangers of an untreated aneurysm.
- Thromboembolism (Clot Throwing): Blood flow inside the aneurysm sac slows down and becomes turbulent. This creates a favorable environment for clots to form inside the sac. Small fragments of these clots can travel through the bloodstream to the legs, kidneys or intestines, where they can clog blood vessels. This can lead to very serious consequences such as sudden and severe pain, loss of function or gangrene in the affected organ.
- Aortic dissection: This is a rarer condition. A small tear develops in the innermost layer of the aortic wall and blood enters through the tear, separating the layers of the wall. This further weakens the wall and increases the risk of rupture, which is itself an emergency.
Pressure on Neighboring Organs: Very large aneurysms can cause chronic back pain by pressing on the spine or nutritional problems by pressing on the organs of the digestive system.
How is Abdominal Aortic Aneurysm Diagnosed?
Today we have very reliable and practical methods for diagnosing an aneurysm. The diagnostic process usually involves these steps:
- Patient History and Physical Examination: First, we listen to the patient’s complaints and inquire about risk factors (smoking, family history, etc.). During abdominal examination, especially in a weak patient, an experienced physician may feel a pulsatile mass around the umbilicus. This is the most common physical examination finding for abdominal aortic aneurysm, but it alone is not sufficient and reliable for the diagnosis.
- Abdominal Ultrasound (USG): It is the most frequently used and first preferred method in diagnosis and follow-up. Since it works with sound waves, there is no radiation risk, it is painless, fast and extremely successful in measuring the presence and extent of the aneurysm. A definitive diagnosis can usually be made in a 10-15 minute procedure.
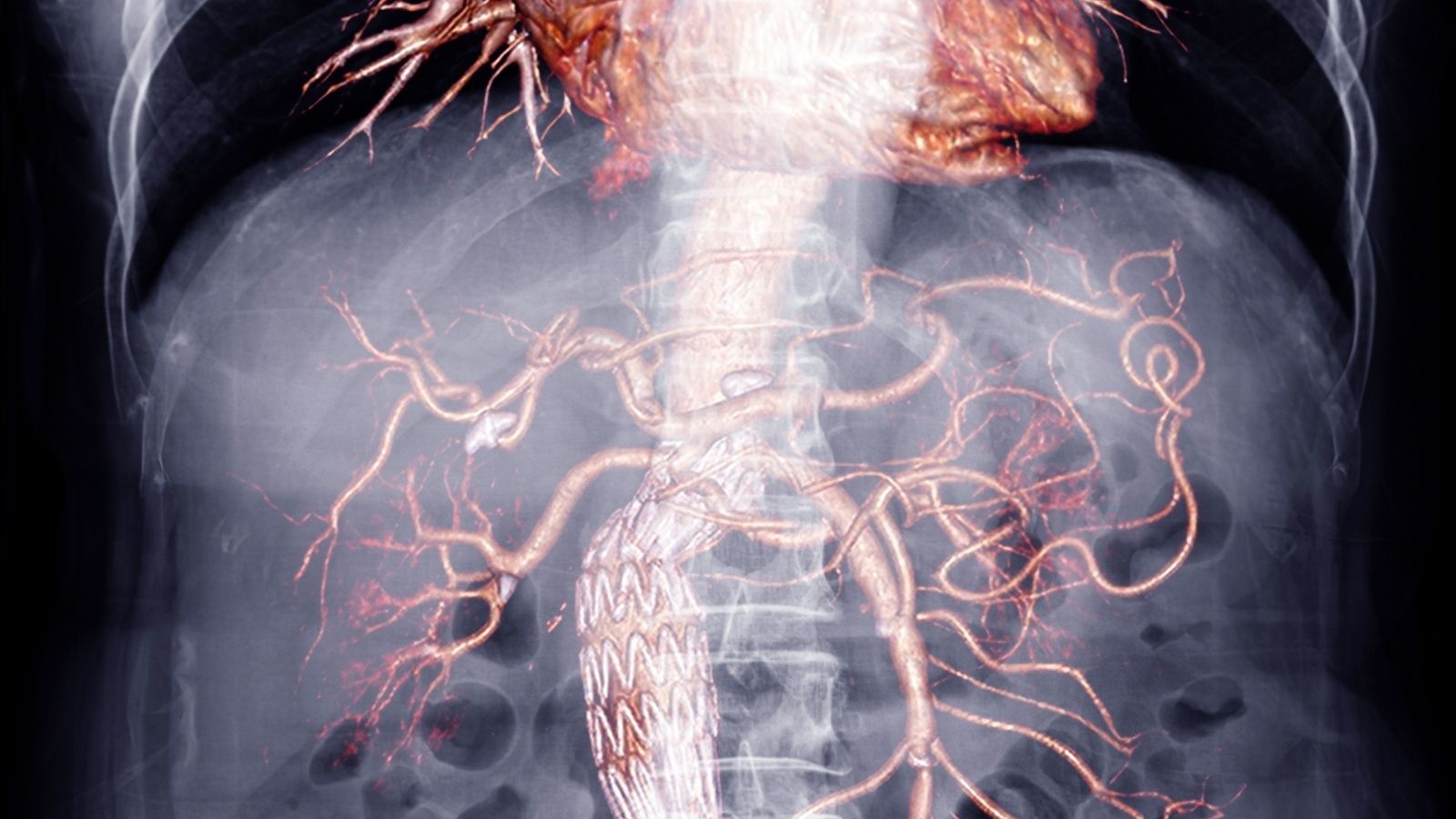
- Computed Tomography (CT) Angiography: This method is the “gold standard” for us, especially when a treatment (surgery) is planned. This CT scan, in which a special dye (contrast dye) is injected into the vein, produces a three-dimensional, highly detailed map of the aneurysm. It gives us critical information such as where the aneurysm starts, where it ends, its relationship to vital side branches such as the renal vessels, and the condition of the vessels leading to the legs. This detailed roadmap allows us to decide which treatment method is the most appropriate and safest for the patient.
Who should be screened for abdominal aortic aneurysm?
Because of the “silent” nature of aneurysms, it is crucial to catch people at risk before they develop symptoms. Screening programs developed for this purpose have a proven success in reducing aneurysm-related deaths.
The screening criteria recommended by international health authorities are very clear.
- Strongly Recommended Group: All men between 65 and 75 years of age who have smoked (or still smoke) in their lifetime. It is recommended that these people should be screened with a one-time abdominal ultrasound, even if they have no complaints.
- Groups that can be evaluated: Men aged 65-75 years who have never smoked but have a family history of aneurysms. Women aged 65-75 years who smoke or have a family history of aneurysms. People in these groups can discuss their personal risk assessment with their doctor and decide together whether screening is right for them.
The goal of the screening program is simple: to catch the aneurysm at a safe stage, before its most dangerous and fatal complication, rupture, occurs. With early diagnosis, regular follow-up and a planned intervention at the right time, it is possible to prevent sudden death due to this disease to a great extent.
What Does “Active Monitoring” Mean for a Small Abdominal Aortic Aneurysm?
Not every patient diagnosed with an aneurysm needs surgery immediately. In fact, most of the time it is not necessary. If the aneurysm is small (usually less than 5.5 cm in men and less than 5.0 cm in women) and does not cause any symptoms, a strategy called “active surveillance” or “medical monitoring” is followed. It is much more than “wait and see”; it is a process in which the patient and the aneurysm are managed closely and proactively.
The main objectives in this process are:
- Monitoring Aneurysm Growth: Regular imaging tests are performed to monitor changes in the size of the aneurysm. This is usually done with abdominal ultrasound because it is safe and practical. Depending on the diameter of the aneurysm, these checks are repeated every 6 months or every 2-3 years.
- Managing Risk Factors Aggressively: This process focuses on the underlying causes to slow the growth of the aneurysm. The patient is advised to give up smoking and to keep their blood pressure and cholesterol under strict control with medication. It is also recommended to avoid activities that can cause sudden increases in blood pressure, such as heavy lifting and straining.
Active surveillance is the safest approach when the risk of rupturing an aneurysm is lower than the risks of major surgery. Thanks to regular check-ups, if the aneurysm reaches a dangerous size or grows faster than expected, we can detect it immediately and proceed to treatment.
When Is Abdominal Aortic Aneurysm Surgery Decided?
The basic principle we use to make the decision to operate is similar to a balance scale. On one side of the scale is the risk of rupture of the aneurysm if left alone, and on the other side is the risk of a planned surgery. At the point when the risk of rupture starts to outweigh the risk of surgery, we make the decision to operate.
There are objective criteria that led to this decision.
- Aneurysm aneurysm: This is the most important criterion. The risk of rupture increases logarithmically as the diameter increases. Generally accepted thresholds are 5.5 cm for men and 5.0 cm for women.
- Growth Rate: Even if the aneurysm has not yet reached the limit of surgery, if it is growing rapidly (e.g. more than 1 cm per year), this is considered a sign that the wall structure is weak and unstable and may lead to the decision to operate.
- Presence of Symptoms: New onset and persistent abdominal or back pain that is thought to be due to an aneurysm, regardless of its size, is usually a sign of an imminent threat of rupture. This requires urgent or very soon planned surgery.
For each patient, this decision is made in consultation with the patient, taking into account his/her specific situation (age, general health status, other concomitant diseases).
What Surgical Options Are Available in the Treatment of Abdominal Aortic Aneurysm?
- Abdominal aortic aneurysm surgery with Y-graft
Today, there are two main surgical methods to treat abdominal aortic aneurysm: Traditional open surgical repair and the more modern method of endovascular aneurysm repair (EVAR).
Traditional Open Surgery Repair:
This technique has been practiced for decades and is considered the “gold standard” with proven long-term success. Under general anesthesia, the aneurysmal aortic segment is accessed directly through an incision in the abdominal wall. The surgeon temporarily stops the blood flow by placing surgical clips in the intact vascular territories above and below the aneurysm. The aneurysm sac is then opened and an artificial vessel (graft) made of a highly durable synthetic material such as Dacron is sewn in place of the diseased and enlarged part of the vessel. This artificial vessel creates a new, smooth and healthy pathway for the blood to flow. After the procedure is finished, the clamps are removed and blood flow is restarted through the new graft.
- Recovery: Open surgery is a major undertaking. Patients stay in intensive care for a few days after surgery, with total hospitalization usually lasting 5 to 10 days. Full recovery and recovery can take 2 to 3 months.
- Risks: As with any major surgery, there are risks of complications involving the heart, lungs and kidneys. There are also risks of bleeding, infection and incision hernia.
Endovascular Aneurysm Repair (EVAR):
EVAR is a minimally invasive, i.e. “closed” method developed in the last two decades. In this technique, the abdomen is not opened. Instead, small incisions or a needle is inserted through arteries in the groin area. Using thin, flexible tubes called catheters, a fabric-covered artificial vessel (stent-graft) with a metal skeleton (stent) is guided into the aneurysm under the guidance of X-ray images. When the stent-graft is deployed inside the aneurysm, it traps the blood flow inside itself. The blood no longer presses against the weak walls of the aneurysm sac, but continues to flow safely directly through the stent-graft. The aneurysm sac, which is released from the pressure, shrinks and shrinks over time.
- Suitability EVAR is not suitable for every patient. The patient’s vascular structure (anatomy) must be suitable for safe stent-graft placement and retention. This suitability is meticulously evaluated with detailed tomographs taken before surgery.
- Recovery Process: The biggest advantage of EVAR is that it offers a much faster and more comfortable recovery process. Patients are usually discharged within 1 to 3 days and can return to their normal life within a few weeks.
- Risks and Follow-up: The most important risk associated with EVAR is endoleak, which is the continued leakage of blood from around the stent-graft into the aneurysm sac. It is therefore imperative that patients who undergo EVAR are followed up regularly throughout life (usually once a year) with ultrasound or CT scanning to ensure that this device is functioning properly.
Which Abdominal Aortic Aneurysm Treatment is Better for You?
This is the most common question asked by our patients and the answer is personalized. There is not a “best” method, but rather a method that is “best for you”. The choice requires a balance between short-term comfort and long-term durability.
Although Open Surgery has a more laborious recovery process, it offers a permanent solution that usually lasts for life and does not require routine follow-up afterwards. It is usually considered primarily in patients who are young, in good general health and have a long life expectancy.
EVAR offers the advantage of lower operative risk and a much faster recovery. It is therefore often a safer option for older patients or those with serious co-morbidities who cannot afford the stress of open surgery. However, this comfort comes with the responsibility of lifelong follow-up and the possibility that additional intervention may be needed in the future.
This decision will be made after a detailed discussion with your surgeon, based on your medical condition, the nature of your aneurysm and your own priorities.
How Does Life Go On After Abdominal Aortic Aneurysm Repair?
| The Progression of Renewal | It may take 2-4 weeks after open surgery and 10-15 days after endovascular (EVAR) intervention. |
| Method of Surgery | Open surgery (graft placement) or endovascular stent graft (EVAR). |
| Physical Activity | Limited activity in the first weeks, then gradual increase; heavy lifting is prohibited for the first 6 weeks. |
| Drug Use | Antihypertensives, aspirin, statins and, if necessary, blood thinners should be taken regularly. |
| Blood Pressure and Cholesterol Control | It is one of the most critical follow-up points; target values are set by the doctor. |
| Imaging and Monitoring | After open surgery, follow-up is usually required once a year; after EVAR, more frequent follow-up (3-6 month intervals with CT angiography) is required. |
| Complications | Risks such as infection, bleeding, graft occlusion in open surgery; endoleak (blood leakage), stent slippage in EVAR. |
| Wound Care | Incision sites should be kept clean and dry; be alert for signs of infection. |
| Nutrition | A balanced diet that promotes vascular health and is low in fat and sodium is recommended. |
| Smoking and Alcohol | Smoking is strictly forbidden; it increases the risk of vascular disease. Alcohol should be consumed in moderation. |
| Sexual Activity | After physical recovery, it is usually possible with doctor’s approval after 4-6 weeks. |
| Psychological Status | Depression/anxiety may occur after a life-threatening situation; support can be sought. |
| Tool Usage | It can usually be started after 4-6 weeks, if attention and physical fitness have been achieved. |
| Controls | Cardiovascular surgery and radiology follow-up should continue regularly throughout life. |
The most basic and most beautiful outcome of a successful aneurysm repair is that it eliminates the risk of the patient suddenly losing his or her life due to an aneurysm rupture. After successful surgery for a planned (unruptured) aneurysm, the long-term life expectancy of patients who survive the critical period, especially the first 3 months, is very close to the life expectancy of the general population in their age and gender group.
After surgery, the vast majority of patients can lead a normal, active and high-quality life. However, there is a very important point to remember: Surgery fixes the “mechanical problem” in your aorta, but does not treat the underlying “arteriosclerosis” that causes this problem. It is therefore vital that you follow certain lifelong precautions to maintain your vascular health after surgery, not only to prevent new aneurysms, but also to improve your overall life expectancy and quality by reducing your risk of other dangerous vascular diseases such as heart attack and stroke.
Here are the basic principles you should follow throughout your postoperative life:
- Avoid smoking and all tobacco products
- Taking blood pressure and cholesterol medications prescribed by your doctor without interruption
- Adopting a healthy and heart-friendly diet
- Keeping your weight in the ideal range
- Do regular, non-strenuous exercise (such as walking).
Frequently Asked Questions
What happens if an abdominal aortic aneurysm ruptures?
An aneurysm rupture is like a burst main artery in the abdomen and starts severe internal bleeding within minutes. Sudden abdominal/back pain, darkening of the eyes, fainting and shock develop. This is one of the most urgent and life-threatening situations in medicine. Getting the patient to the hospital as quickly as possible and emergency surgery saves lives.
Is abdominal aortic aneurysm surgery risky?
Every major surgery has risks, but in planned surgery before the aneurysm ruptures, the risk is quite low. In emergency, post-rupture surgery, the risk is much higher. We minimize this risk with early diagnosis and planned surgery.
How many hours does abdominal aortic aneurysm surgery take?
Open surgery usually takes 3-4 hours, while the closed (endovascular) method takes an average of 2 hours. Every patient is different, but the important thing is that the procedure is safe and successful rather than the duration.
Which doctor treats abdominal aortic aneurysm?
Cardiovascular Surgeons are responsible for the diagnosis, follow-up and treatment of this disease. The diagnosis is sometimes made incidentally by radiology, but treatment and follow-up must be carried out by this specialty.
Risk of death after aortic aneurysm surgery?
The risk of death in planned operations without rupture is 2-5% in experienced centers. In emergency operations performed after the aneurysm is ruptured, this rate rises to @-50%. The importance of early diagnosis and timely surgery is hidden here.
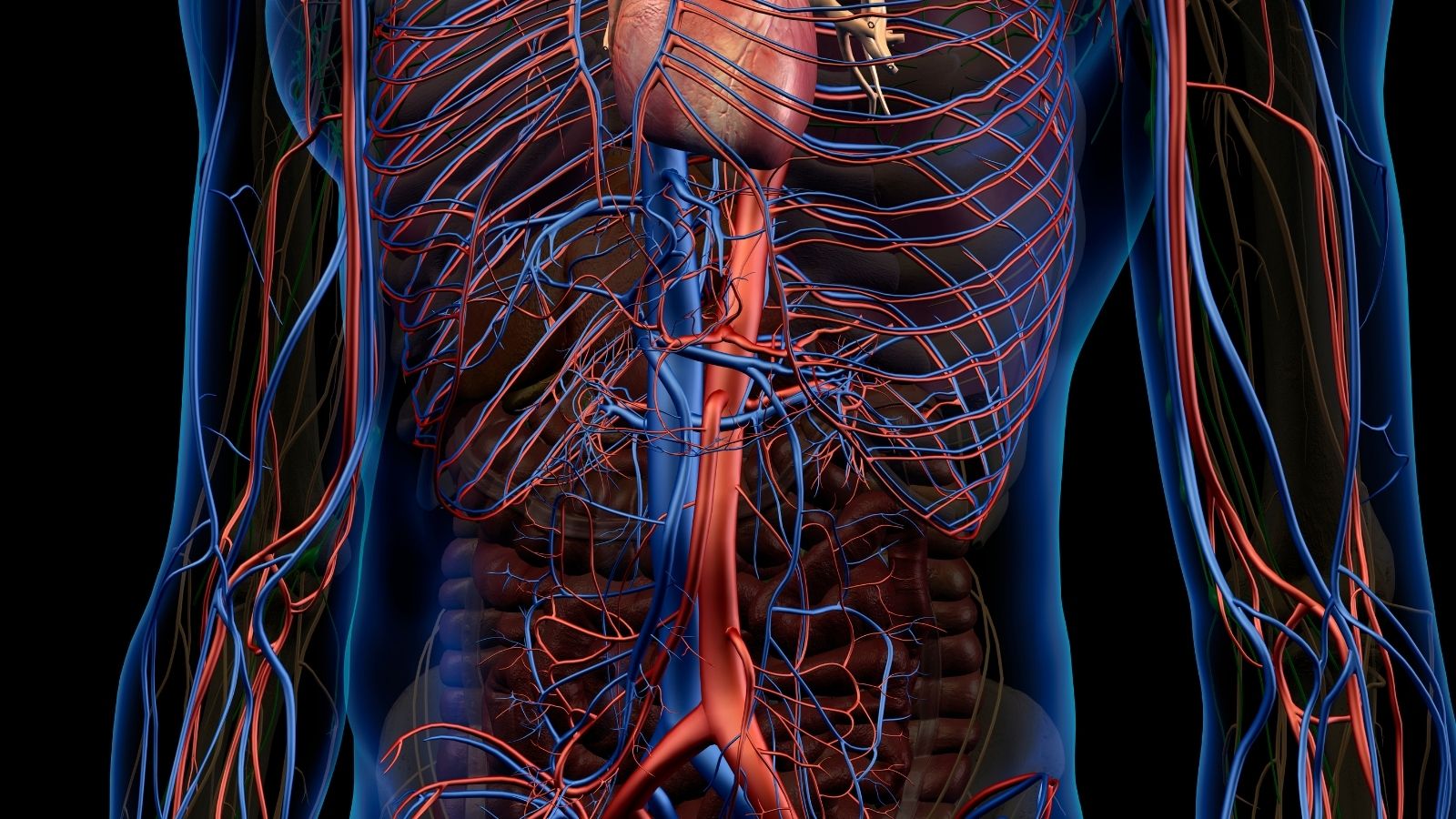
Where is the aorta in the abdomen?
The aorta is located in the abdominal cavity just anterior to the spine, usually at the level of the navel. It is the main artery of the body that distributes blood to all the abdominal organs and limbs.
Where is an abdominal aortic aneurysm most common?
It is most common in the section of the aorta after the renal arteries (infrarenal region), slightly below the umbilicus. Aneurysms occur in this region.
What is abdominal aortic aneurysm repair?
A rupture is a rupture of the wall of the aneurysm. When the vessel wall becomes thinner and balloons, it cannot withstand the pressure and bursts, causing sudden bleeding into the abdomen. This condition becomes life-threatening very quickly and requires urgent intervention.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.