The human heart is a muscular organ responsible for pumping oxygenated blood to the body and deoxygenated blood to the lungs. It consists of four chambers, valves, and a conduction system that ensures rhythmic contractions and efficient circulation.
The right atrium and ventricle manage pulmonary circulation, sending deoxygenated blood to the lungs. The left atrium and ventricle handle systemic circulation, delivering oxygen-rich blood to organs and tissues throughout the body.
Heart valves, including the mitral, tricuspid, aortic, and pulmonary valves, regulate unidirectional blood flow. Malfunction of these valves can lead to significant clinical conditions such as stenosis or regurgitation, affecting overall cardiac performance.
The cardiac conduction system, composed of the sinoatrial node, atrioventricular node, and His-Purkinje fibers, coordinates electrical impulses. This ensures synchronized contractions, maintaining stable heart rhythms essential for life.
What is our heart and what are its main functions?
Our heart is the center and the hardest working organ of our circulatory system. It works like a pump in its muscular structure, delivering blood through the blood vessels to the most remote corners of our body. This seemingly simple pumping function actually fulfills a number of critical tasks for the continuation of life. The heart’s functions make it the most important organ in our body.
The most basic tasks of the heart can be summarized under a few headings:
- Transport oxygen and nutrients to tissues
- Collecting waste products generated in cells
- Helping the body fight infections
- Delivering hormones to the relevant organs
- Contributing to body temperature stabilization
Our heart is located in the center of our rib cage, between our two lungs, just behind the sternum, also known as the faith board. This protected position alone shows how precious it is. If this pump stops working for a moment, it can cause irreversible damage within seconds, especially to the brain, our most oxygen-sensitive organ. Therefore, maintaining heart health is not a choice but a necessity. The heart’s “double pump” system, which sends dirty blood to the lungs to be cleaned and distributes clean blood throughout the body, is a marvel of highly efficient engineering. When the delicate balance between these two circulations is disturbed, for example when there is a hole between the chambers of the heart, the entire efficiency of the system is reduced and the heart has to work many times harder than normal. This sets the stage for heart failure over time.
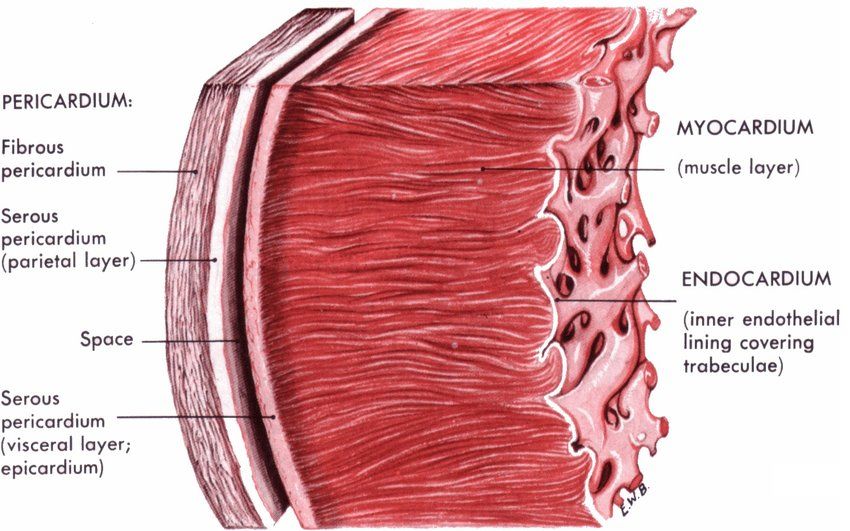
What is the Structure of the Layers Forming the Wall of the Heart?
If we compare our heart to a building, the walls of this building are made of three layers of different materials, each serving a different purpose. The heart structure is both protected and fully functional thanks to the harmonious union of these three layers from the outside to the inside.
These three basic layers that make up the heart wall are:
- Pericardium
- Myocardium
- Endocardium
The pericardium is a double-layered membrane that surrounds the heart like an outer pouch. The outer leaf is harder and more durable, while the inner leaf is slippery. The small amount of fluid between the two leaves prevents the heart from friction with each beat, allowing it to move freely. The pericardium stabilizes the heart in place, prevents it from over-expanding and acts as a shield against infections. When this membrane becomes inflamed (pericarditis), there is a sharp chest pain that can often be mistaken for a heart attack. During heart surgery, surgeons need to open this sac to access the heart.
The myocardium is the thickest and most functional layer of the heart wall; in short, it is the muscle of the heart. It is this layer that provides the pumping power of the heart. In particular, the myocardium of the left ventricle, which is responsible for pumping blood throughout the body, is significantly thicker than the rest of the heart. This thickness is necessary to work against higher pressure. A heart attack caused by a blockage in the coronary arteries means that part of this muscle layer is directly deprived of oxygen and dies. Damage to this area can permanently reduce the heart’s ability to contract.
The endocardium is a thin, smooth lining that lines the inner surface of all the chambers and valves of the heart. This smoothness is critical for blood to flow without sticking or clotting. The heart valves are actually an extension of this endocardium. Therefore, conditions such as inflammation of the endocardium (infective endocarditis) damage the heart valves the most. When bacteria become lodged in this layer, it can lead to severe damage to the valves, perforations and eventually valve failure. This is a serious condition that usually requires long-term antibiotic treatment or surgical repair or replacement of the damaged valve.
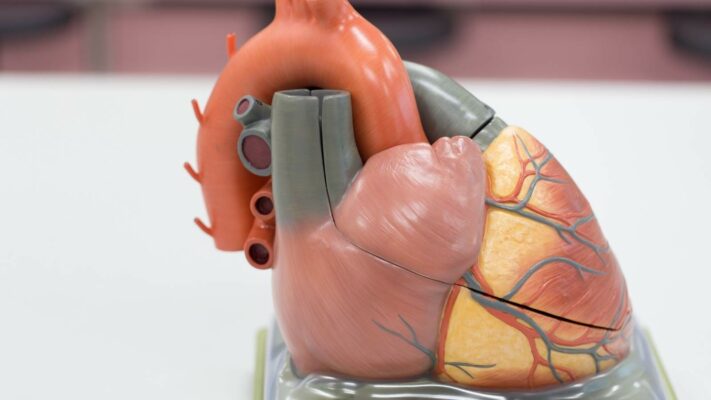
What are the chambers of the heart and how do they work?
Our heart is not an empty organ; it is like a house with four specialized chambers to collect and pump blood. The chambers of the heart, two at the top and two at the bottom, ensure that the blood circulates in the correct order.
The heart has four main chambers:
- Right Atrium (Right Atrium)
- Left Atrium (Left Atrium)
- Right Ventricle (Right Ventricle)
- Left Ventricle (Left Ventricle)
The atria at the top are like waiting rooms that collect blood. The right atrium collects “dirty” blood that has been used in the body and has lost oxygen. The left atrium collects oxygen-rich “clean” blood that has been cleaned in the lungs. When the atria are full, they contract, emptying blood into the ventricles, the larger and stronger chambers just below them.
The ventricles at the bottom are the main pumps of the heart. The right ventricle takes dirty blood from the right atrium and pumps it to the lungs to be cleaned. Because this requires a relatively short distance and low pressure, the walls of the right ventricle are thinner. The left ventricle, on the other hand, receives the clean blood from the left atrium and contracts with tremendous force to pump it all over the body, from the brain to the toes, through the main artery called the aorta. Because of this challenge, the muscle layer (myocardium) of the left ventricle is much thicker and stronger than all the other chambers and parts of the heart.
The walls (septum) separating these chambers ensure that clean and dirty blood do not mix. However, sometimes these walls can be congenitally perforated. Holes between the atria are called ASDs and holes between the ventricles are called VSDs. These holes usually cause blood to leak from the high-pressure left side to the low-pressure right side, or “shunting”. This increases the load on the heart and can lead to increased pressure in the lung vessels. These holes, which are symptomatic or large, need to be closed surgically with a patch or, in some suitable cases, with an umbrella-like device inserted through the groin.
What is the role of the heart valves that manage blood flow?
The heart valves, the gates between the chambers of our heart and at the mouth of the large arteries that exit the ventricles, are perfectly designed to ensure that blood flow is one-way. The heart’s job is to pump blood forward and these valves ensure that this task is done efficiently by preventing blood from escaping backwards.
Our heart has four main valves that manage blood flow:
- Tricuspid Valve
- Pulmonary Valve
- Mitral Valve
- Aortic Valve
The tricuspid valve is located between the right atrium and the right ventricle. The pulmonary valve is between the right ventricle and the pulmonary artery. These two valves manage the circulation of dirty blood. The mitral valve is located between the left atrium and the left ventricle. The aortic valve is between the left ventricle and the main artery (aorta) that carries blood throughout the body. Both control the flow of clean blood. These valves are made up of thin, flexible but robust leaflets that passively open and close in response to changes in pressure inside the heart chambers.
Over time, however, these valves can wear out, calcify or become damaged by infections or diseases such as rheumatic fever. This raises two fundamental problems:
- Stenosis (Stenosis)
- Regurgitation (Regurgitation)
In the case of stenosis, the valve cannot open fully and the heart has to exert much more force to push the blood through the narrow door. In case of insufficiency, the valve cannot close completely and some of the blood pumped forward leaks backwards. This means that the heart has to pump both the blood it needs to pump forward and the blood that has escaped backwards, doubling its workload.
When this type of valve disease progresses, medication may be inadequate and surgical intervention is required. There are several options for surgical treatment. Whenever possible, especially for mitral valves, repairing the patient’s own valve (valve repair) is the first choice. If repair is not possible, the damaged valve is removed and replaced with a mechanical or biological prosthetic valve (valve replacement). In recent years, minimally invasive methods such as valve replacement (TAVR) or repair (MitraClip) through the groin have also become widespread, especially for elderly patients at high risk of open heart surgery.
The Journey of Blood in the Heart and How Does the Circulatory System Work?
The journey of blood through our body is a perfectly organized cycle that never stops. At the center of this cycle is the heart, which determines the direction of the blood and provides the driving force. Following the steps of the blood flow gives the clearest idea about the work of the heart and the circulatory system.
The journey of blood between the heart and lungs follows these steps:
- Blood contaminated in the body enters the right atrium of the heart through two large main veins (vena cava).
- The right atrium contracts and pushes the blood through the tricuspid valve into the right ventricle.
- With a strong contraction, the right ventricle pumps the blood through the pulmonary valve and into the pulmonary artery.
- In the lungs, the blood releases carbon dioxide and takes in oxygen, i.e. it is cleansed.
- The cleansed blood returns to the left atrium of the heart via the pulmonary veins.
- The left atrium contracts and empties the blood through the mitral valve into the left ventricle.
- The left ventricle, the heart’s most powerful chamber, pumps this clean blood through the aortic valve, into the aorta and from there throughout the body.
This cycle forms two main circulatory systems. The one in which the right heart pumps blood to the lungs is called the pulmonary circulation. This is a low-pressure system whose sole purpose is to clean the blood. The left heart pumps clean blood throughout the body and is called the systemic circulation (body circulation). Blood must be at high pressure to reach these organs.
In some complex congenital heart diseases, these pathways may be misconnected or underdeveloped. For example, in cases such as “transposition of the great arteries”, where the aorta and pulmonary artery are switched, dirty blood is constantly pumped into the body and clean blood is constantly pumped into the lungs. This is incompatible with life and requires urgent surgical correction. In such complex cases, surgeons aim to restore normal anatomical blood flow by relocating vessels, creating new pathways (shunts) or patching holes.
How does the heart work through its own electrical system?
The rhythmic and regular contraction and relaxation of the heart is not caused by an external command, but by a specialized electrical impulse and conduction system within the heart itself. This system works like the heart’s natural pacemaker, initiating each beat and ensuring that this impulse is spread regularly throughout the heart muscle. Perfect heart function depends on the health of this system.
The main structures that make up the heart’s electrical conduction system are:
- Sinoatrial Node (SA Node)
- Atrioventricular Node (AV Node)
- His Bundle
- Purkinje Fibers
It all starts when the SA Node, located at the top of the right atrium, generates an electrical signal. This structure is the heart’s natural battery and in a normal person it emits between 60 and 100 regular impulses per minute. This signal first spreads to the atria, causing them to contract. The signal then travels to the AV Node, which acts as a junction between the atria and ventricles. The AV node waits a fraction of a second before transmitting the signal to the ventricles. This critical delay gives the atria time to empty their blood completely into the ventricles.
After this pause, the impulse is rapidly transmitted to the entire ventricular muscle tissue via the bundle of His and then the network of Purkinje Fibers. This fast and synchronized transmission allows the ventricles to contract as a whole and strongly, pumping blood into the lungs and throughout the body. Any disruption in this system leads to rhythm disturbances (arrhythmias). Problems in this system can cause the heart to work too slowly (bradycardia), too fast (tachycardia) or irregularly (such as atrial fibrillation).
Various methods are used to treat rhythm disorders:
- Medicines that regulate rhythm or control speed
- Catheter ablation that burns or freezes the abnormal foci causing the arrhythmia
- Pacemakers that produce a warning when the heart slows down
- Special pacemakers (ICD) that detect life-threatening fast rhythms and correct them with a shock
How Does the Heart Get Its Nutrients from the Coronary Circulation?
Although the heart is an organ that pumps blood throughout the body, it cannot feed on the rich blood that passes through it. Just like any other organ, the heart muscle needs oxygen and nutrients to keep working. It meets this need with its own special vascular network, the coronary circulatory system, which surrounds it like an outer crown.
The main arteries supplying the heart consist of two main branches that emerge from the beginning of the aorta:
- Right Coronary Artery (RCA)
- Left Main Coronary Artery (LCA)
The right coronary artery usually supplies the right side and lower wall of the heart. The left main coronary artery divides into two large branches after a short course: The LAD and LCX. Because the LAD artery supplies a very large and critical area, such as the anterior face of the heart, a complete blockage in this artery usually causes a massive heart attack. These coronary vessels branch deep into the heart muscle, delivering oxygen and nutrients to each muscle fiber.
Coronary Artery Disease, the most common heart disease, is the narrowing or blockage of these arteries over time due to plaques formed by the build-up of cholesterol, fat and calcium on their inner walls. This condition, also known as arteriosclerosis, reduces blood flow to the heart muscle. When the heart needs more oxygen during exertion, this narrowed blood vessel cannot supply enough blood, causing “angina”, which is felt as pressure, tightness or pain in the chest. If one of these plaques suddenly ruptures and a clot forms and completely blocks the blood vessel, a heart attack (myocardial infarction) occurs.
The gold standard for the diagnosis of coronary artery disease is coronary angiography. There are several different approaches to treatment:
- Lifestyle changes such as healthy eating, exercise, smoking cessation
- Blood thinners, cholesterol-lowering and blood pressure regulators
- Expansion of the narrowed vessel with a balloon during angiography and placement of a metal cage called a stent (Percutaneous Coronary Intervention)
If multiple vessels are severely stenotic or not suitable for stenting, new blood vessels from elsewhere in the body are used to create new pathways (bridges) that carry blood beyond the blocked area (Coronary Artery Bypass Surgery)
How are problems in the heart structure diagnosed?
In order to treat heart disease properly, problems and dysfunctions in the heart’s structure must first be accurately diagnosed. Today, there are many technological diagnostic methods that allow us to examine both the structure and function of the heart in detail. The process usually starts with listening to the patient’s complaints and continues with a series of tests.
Commonly used methods for the diagnosis of heart disease include the following:
- Echocardiography (ECHO)
- Electrocardiogram (ECG)
- Effort Test (Stress Test)
- Holter Monitoring
- Coronary Angiography
- Cardiac Magnetic Resonance (MRI) and Computed Tomography (CT)
Echocardiography (ECHO) is a painless and harmless method in which moving images of the heart are obtained using sound waves (ultrasound). This test, which is almost like an ultrasound of the heart, provides vital information such as the thickness of the heart chambers and walls, the strength of contraction, the structure of the heart valves, possible leaks or stenosis and the presence of fluid in the heart membrane. It is the cornerstone of cardiac surgery planning.
An electrocardiogram (ECG) is the most basic test that documents the electrical activity of the heart. It is used to detect rhythm disturbances, a previous or current heart attack and problems with the heart’s electrical conduction system. An exertional test aims to detect problems that occur especially with exertion, by taking an ECG while the patient walks on a treadmill. If the rhythm disturbance only occurs at certain times of the day, a Holter device that records ECGs for 24 hours or longer can be implanted.
Coronary angiography is the “gold standard” method for visualizing coronary vessels. A thin tube (catheter) is inserted into the groin or arm, a special dye is injected into the coronary arteries and X-rays are taken. This allows the location and degree of stenosis to be clearly identified. Cardiac MRI and CT are high-tech methods that provide much more detailed, three-dimensional and cross-sectional images of the heart and large vessels. They are especially used to evaluate more complex conditions such as congenital heart disease, the viability of heart muscle tissue or heart tumors. These tests are evaluated as a whole and the most appropriate treatment plan (medication, stent or surgery) is determined by the “heart team”.
Frequently Asked Questions
What is the heart and what does it do?
The heart is a muscular organ located in the chest that pumps blood continuously. It carries oxygen and nutrients to all organs of the body.
How many chambers does the heart have?
The heart has four chambers: Two atria (atria) and two ventricles (ventricles).
Are there valves inside the heart?
Yes, there are four main valves – mitral, tricuspid, aortic and pulmonary – that keep the blood flowing in the right direction.
What is the structure of the heart?
The heart is made up of three main layers: Endocardium (inner layer), myocardium (muscle layer) and pericardium (outer membrane layer).
Is the heart muscle different from other muscles?
Yes, the heart muscle (myocardium) is a special type of muscle that works involuntarily and is capable of generating electrical impulses on its own.
How does the heart work?
The heart contracts by electrical signals and pumps blood from the atria to the ventricles and then to the veins. This system is called the cardiac cycle.
What is the system that controls how the heart works?
The “sinus node” initiates the heartbeat. This structure acts like the heart’s natural pacemaker.
How many beats per minute does the heart beat?
In a normal adult, the heart beats 60-100 times per minute. In athletes, this number may be lower.
How is the heart muscle nourished?
The coronary arteries that supply the heart carry oxygen and nutrients to the heart muscle.
What causes the heart to fail?
When the heart is unable to pump blood sufficiently, conditions such as heart failure, arrhythmias or shock can occur.
How is blood flow in the heart?
Dirty blood enters the right atrium, passes to the right ventricle and is sent to the lungs. The cleansed blood is pumped through the left atrium and left ventricle.
Why does the heart work both ways?
The right side sends blood to the lungs, while the left side pumps clean blood throughout the body. This double circuit system is vital.
How to listen to the heart?
The heart rests for short periods of milliseconds between each beat. These short moments of rest are very precious for the heart muscle.
Does the structure of the heart change?
Yes, conditions such as hypertension, heart disease, exercise can thicken the walls of the heart or widen the chambers.
How to maintain heart health?
A healthy diet, regular exercise, avoiding smoking and stress, and keeping blood pressure and cholesterol under control are important for heart health.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.