Mitral valve prolapse (MVP) occurs when the valve leaflets bulge backward into the left atrium during heart contraction. This condition is relatively common and often benign, but in some cases may cause regurgitation or arrhythmias.
Symptoms of MVP include palpitations, chest pain, dizziness, and fatigue. Some patients may remain asymptomatic, while others experience worsening shortness of breath or anxiety, particularly when valve leakage becomes significant.
Complications associated with mitral valve prolapse include infective endocarditis, progressive mitral regurgitation, and in rare cases sudden cardiac events. Echocardiography remains the gold standard for diagnosis and monitoring.
Treatment depends on severity, ranging from observation in mild cases to beta-blockers for symptoms, and surgical repair or replacement for advanced valve regurgitation. Regular follow-up is essential to track progression.
| Medical Term | Mitral valve prolapse (MVP) |
| Definition | Prolapse of the mitral valve between the left atrium and left ventricle into the atrium during ventricular systole |
| Frequency of Appearance | 2 to 3% in the general population |
| Main Causes | Idiopathic (mostly), Marfan syndrome, Ehlers-Danlos syndrome, rheumatic valve disease |
| Symptoms | Asymptomatic in most cases â In some patients, chest pain, palpitations, dizziness, dyspnea, shortness of breath |
| Physical Examination Finding | Midsystolic click and/or late systolic murmur |
| Diagnostic Methods | Echocardiography (M-mode and 2D), ECG (for the presence of arrhythmia), Holter monitoring |
| Complications | Mitral regurgitation, atrial fibrillation, endocarditis, rarely sudden cardiac death |
| Treatment Methods | Follow-up in mild cases â If there are symptoms: beta-blockers, antiarrhythmics â Surgery in severe mitral regurgitation (valve repair or replacement) |
| Tracking Process | Regular echocardiographic monitoring, especially in patients with mitral regurgitation |

Prof. Dr. Yavuz Beşoğul
>Turkey’s Cardiovascular Surgery Doctor
What is Mitral Valve Prolapse?
 Mitral Valve Prolapse[/caption
Mitral Valve Prolapse[/caption
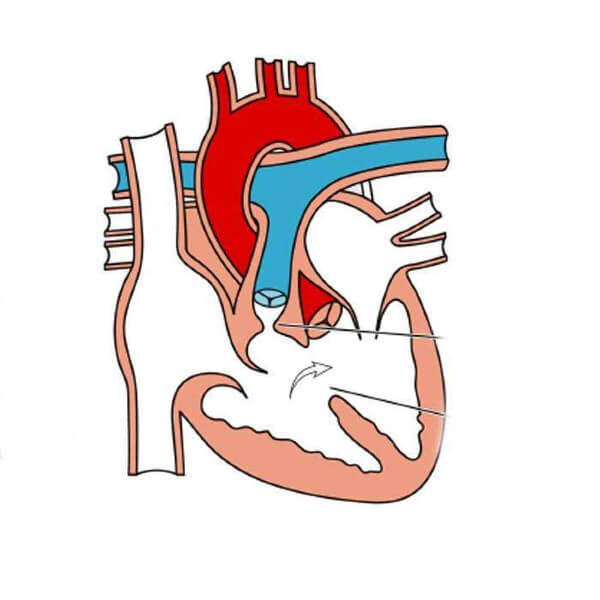
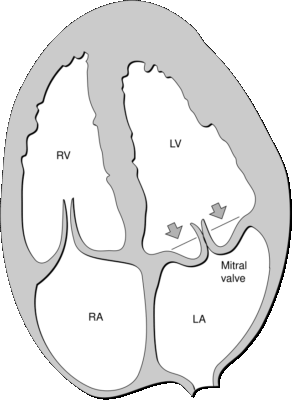
Inside our heart there are four valves that keep the blood flowing in the right direction. The mitral valve is a two-leaf valve located between the upper chamber (left atrium) and the lower chamber (left ventricle) on the left side of the heart. Its function is to allow clean blood from the lungs to pass from the left atrium to the left ventricle, and then to close tightly to prevent the blood from backing up as the left ventricle contracts and pumps this blood into the body.
In mitral valve prolapse, the leaflets of this valve are slightly more flexible and loose than normal. Therefore, when the heart contracts, one or both of the valves bulges slightly backwards into the left atrium. This can be likened to the slight upward yawn of an avalanche on a rail. Most of the time this flexing is insignificant and does not disrupt the functioning of the closure. In some cases, however, this bulging can prevent the valve from closing and cause a small amount of blood to leak backwards into the left atrium with each heartbeat. In medical language, this condition is called “mitral regurgitation” or “mitral regurgitation”.
How common is Mitral Valve Prolapse?
Mitral valve prolapse is a much more common condition than is commonly believed and is thought to affect approximately 2-3% of the general population. It can occur in any age and gender. However, severe symptoms or progression of valve insufficiency are slightly more common in men over 50.
In the past, when imaging methods such as echocardiography were less sophisticated, this rate was reported to be much higher, even reaching 0. This was because the old technology was unable to assess the normal and healthy three-dimensional structure of the valve and interpreted even the slightest backward movement as a prolapse. Today, with modern echocardiography equipment and clearer diagnostic criteria, the true prevalence of the condition is more accurately known. Clear measurements, such as the valve bulging over a certain distance, are now used to diagnose a person with prolapse.
What causes Mitral Valve Prolapse?
The most common underlying cause of mitral valve prolapse is an innate feature in the connective tissue of the valve. This makes the valve leaflets more flexible and thicker than normal. There is often a familial predisposition, meaning that if parents have it, children are more likely to have it. The causes generally fall into two main categories.
The first is “Primary Mitral Valve Prolapse”, where the problem is directly in the structure of the valve itself. This is the most common form and is related to a process known in medical parlance as “mixed degeneration”. Basically, the spongy tissue inside the lid weakens and thickens over time, leading to sagging.
The second is “Secondary Mitral Valve Prolapse”. In this case, the valve leaflets are actually normal, but another heart condition causes them to prolapse. This can be caused, for example, by damage to the muscles that hold the valves after a heart attack.
In addition, mitral valve prolapse is closely associated with certain hereditary connective tissue diseases. Some of these diseases include the following:
- Marfan syndrome
- Ehlers-Danlos syndrome
- Graves’ disease
- Scoliosis
- Muscular dystrophy
What symptoms can Mitral Valve Prolapse cause?
A very large proportion of people with mitral valve prolapse do not experience any symptoms throughout their lives. Most of the time, it is discovered accidentally during a doctor’s examination for another reason. When symptoms do appear, they can vary from person to person. Common symptoms include the following:
- Distortion
- Shortness of breath (especially on exertion or lying down)
- Atypical chest pain (different from the pain of a heart attack, stabbing or sudden)
- Constant fatigue and weakness
- Dizziness or feeling dizzy
It is important to emphasize one very important point: the severity of symptoms is not always directly proportional to the severity of the valve problem. A person with a very mild valvular valve may experience severe palpitations that impair quality of life, while another person with severe valve insufficiency may be completely asymptomatic. This is thought to be due to an imbalance of the autonomic nervous system that can accompany prolapse. Sometimes these symptoms can be so intense that mitral valve prolapse can trigger a panic attack-like condition. The sudden onset of palpitations, breathlessness and chest pain can cause intense fear and anxiety. The presence of symptoms alone is therefore not a danger sign, but should always be evaluated by a cardiologist.
How is Mitral Valve Prolapse diagnosed?
The process of making the diagnosis of mitral valve prolapse usually involves several steps and is quite simple.
The first step is usually for the doctor to examine you and listen to your heart with a stethoscope. The classic sign of prolapse is a sharp “click” as the heart contracts, stretching the prolapsed valves. If there is also a leak in the valve, this is accompanied by an innocent “murmur” sound made by the blood as it recedes.
The most important test to confirm the diagnosis and determine the severity of the condition is echocardiography. This test, known simply as “ECHO”, is an ultrasound of the heart. It uses sound waves to create moving images of your heart and valves. With this test, the following can be clearly seen:
- Whether prolapse is present
- Structure and thickness of the covers
- Degree of valvular heart valve (mitral regurgitation), if any
- Dimensions of the heart chambers and the strength of the heart muscle
Usually a standard ECHO through the chest is sufficient. Sometimes, especially in cases such as surgery planning, a transesophageal ECHO (TEE) through the esophagus may be needed to obtain clearer images. Additional tests such as ECG (electrocardiogram) may also be ordered to evaluate rhythm disturbances.
What serious consequences can mitral valve prolapse lead to?
First of all, it should be noted: For the vast majority of patients with mitral valve prolapse, the condition is benign and causes no serious problems throughout life. Complications are rare, but it is useful to know these risks to understand why regular follow-up is important.
The most common complication is that the leak in the valve, mitral regurgitation, increases over time. A mild leak can become severe over the years. Severe regurgitation causes the heart to work harder and harder to pump blood around the body, which can lead to heart failure if left untreated.
Another possible complication is heart rhythm disorders (arrhythmias). The most common is Atrial Fibrillation, which causes the heart to work irregularly and rapidly. This arrhythmia can predispose to the formation of clots inside the heart and the risk of stroke.
In recent years, it has been recognized that in a very small and special group of patients, life-threatening arrhythmias can develop even in the absence of severe valve disease. because of this rare condition, termed “arrhythmogenic MVP”, the risk of sudden death from mitral valve prolapse is occasionally raised. However, it is important to emphasize that this risk does not apply to the overwhelming majority of patients with prolapse, but only to a very specific subgroup with certain ECG and MRI findings. Patients with complaints such as fainting should be carefully evaluated in this respect.
Does every case of Mitral Valve Prolapse require treatment?
Absolutely not. People who are asymptomatic and have no significant valve problems do not need treatment. The best approach for these people is to have regular cardiology check-ups to monitor the situation at regular intervals. This follow-up process is called “watchful waiting” and usually involves repeated echocardiography tests every few years.
If symptoms such as palpitations are impairing quality of life, medication may be used to control these symptoms. The most commonly used drugs for this purpose are beta-blockers. These drugs are very effective at slowing the heartbeat and reducing symptoms such as palpitations and chest pain. However, it should be remembered that medications do not correct the underlying problem with the valve, only the symptoms.
What should people with Mitral Valve Prolapse pay attention to?
The answer to the question of what to do if you have mitral valve prolapse depends on the severity of the condition, but it is in everyone’s best interest to adopt a heart-friendly lifestyle. General recommendations are as follows:
- Regular Exercise: There are no exercise restrictions for most people with mild prolapse. Activities such as walking, swimming and cycling are encouraged. Those with severe valvular insufficiency should consult their doctor before practicing heavy and competitive sports.
- Healthy Diet: Adopting a diet low in salt, processed foods and saturated fats and rich in vegetables and fruits will ease the burden on your heart.
- Weight Control: Maintaining a healthy weight allows your heart to work more easily.
- Stress Management: Relaxation techniques such as yoga and meditation can help manage stress, which can trigger symptoms, especially palpitations.
- Avoiding Stimulants: Substances such as caffeine, alcohol and cigarettes can increase palpitations in sensitive people. Limiting or eliminating these products may help.
- Oral and Dental Hygiene: Good oral hygiene and regular dental check-ups are important to minimize the risk of valve infection (endocarditis).
When is surgery necessary for mitral valve prolapse?
The decision to operate is based on the severe mitral regurgitation caused by the prolapse, not the prolapse itself. Surgical intervention becomes necessary in the following cases.
Presence of Symptoms: If you have started to experience shortness of breath and fatigue due to severe valvular heart disease, this is a clear need for surgery.
The Onset of Heart Damage Even Without Symptoms: This is the most critical and sometimes the most difficult to understand. A person may wonder why they need surgery when they feel fine. The answer is to intervene before permanent damage to the heart occurs. Serious valve leakage creates a burden on the heart that lasts for years. The heart gets bigger and works harder to meet this load, so for a long time the person feels no symptoms. At some point, however, the heart muscle gets tired and weakens. If surgery is performed after this permanent damage has occurred, heart function may not be the same even if the valve is repaired.
Therefore, even if you have no symptoms, if echocardiography shows a decrease in the pumping power of the heart or enlargement of the heart chambers, surgery is proactively recommended to preserve the heart muscle.
What is the difference between repair and replacement in mitral valve prolapse surgery?
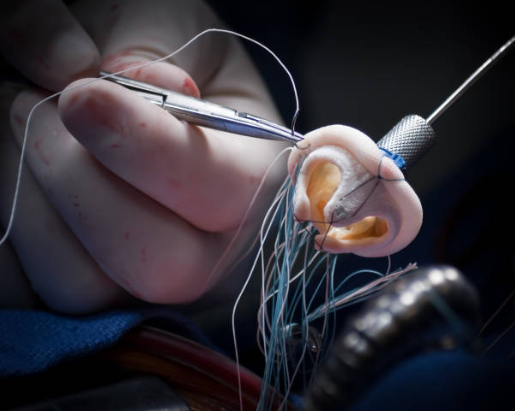
When surgery is needed, there are two main options. Cover repair or cover replacement.
- Valve Repair (Repair): In this procedure, the surgeon preserves the patient’s own valve tissue to repair it and make it function normally again. The prolapsed parts are straightened, excess tissue is removed and the ring in which the valve sits is reinforced with a support ring (an annuloplasty ring). In experienced centers, more than one percent of valve regurgitations due to prolapse can be successfully repaired.
- Valve Replacement: If the valve is damaged beyond repair, it is removed and replaced with an artificial (prosthetic) valve.
Whenever possible, valve repair is definitely preferable to valve replacement. Because repair surgery has better outcomes, preserves heart function better and, most importantly, eliminates the need for the patient to take blood thinners for life.
What are the modern surgical methods for Mitral Valve Prolapse?
Today, mitral valve surgeries are performed with advanced technologies that maximize patient comfort. Instead of traditional open heart surgery, methods such as minimally invasive and robotic surgery have come to the fore.
Minimally Invasive Surgery: In this method, the chest bone is not cut. The heart is accessed through a small incision of about 4-6 cm on the right side of the chest, between the ribs.
Robotic Surgery: The most advanced form of minimally invasive surgery. From a console, the surgeon manages robotic arms that are inserted through several small holes in the chest. This technology offers the possibility to make movements under a three-dimensional and magnified image, much more precise than the human hand.
These modern techniques have many advantages over traditional surgery:
- Faster recovery
- Less pain
- Shorter hospitalization
- Less blood loss and risk of infection
- Better cosmetic results
These advanced techniques require a high level of experience and the best results are obtained in centers where these surgeries are frequently performed.
Frequently Asked Questions
Is mitral valve leakage dangerous?
It is usually not a disease to be feared. In most people, mitral valve leakage causes no symptoms and does not affect quality of life. It only becomes important in very rare advanced cases if severe blood clots develop. Regular medical check-ups are sufficient; no need to worry!
What should people with a burst heart valve do?
First of all, stay calm and check regularly with your cardiologist. Your doctor will monitor the relaxation of the valve and possible valve rupture with an echocardiogram. A healthy lifestyle (plenty of water, stress management, limiting caffeine and alcohol) will reduce your symptoms. Get information from your doctor; do not believe all the information on the internet.
What causes mitral valve prolapse?
Most of the time it does not cause any symptoms. Some patients may have palpitations, stinging in the chest, shortness of breath or dizziness. In rare cases, if a severe valve develops, there may be âmitral insufficiencyâ. But there is no rule that this will happen in every patient.
Does a heart valve collapse prevent military service?
In mild cases and unless there is a serious heart or rhythm disorder, it is usually not a disability. If there is severe to severe toeing, significant heart disease or dangerous arrhythmias, it may be grounds for exemption from military service. The cardiologist at the military hospital makes the final decision.
Does a heart valve flutter?
Yes, fluttering is the most common complaint of mitral valve collapse. A loose valve can stimulate the heart’s electrical system and cause innocent extra beats. It is mostly harmless; if it reduces your quality of life, it can be controlled with medication.
Is mitral valve prolapse genetic?
Yes, genetic predisposition is common. People with first-degree relatives with mitral valve prolapse have an increased risk of developing it. This is because the connective tissue is inherently looser. It is often a family trait.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.