Myocardial bridging is a congenital heart anomaly where a segment of a coronary artery tunnels through the heart muscle instead of lying on its surface. This can cause compression during heart contractions, potentially leading to reduced blood flow.
Symptoms of myocardial bridging may include chest pain, palpitations, dizziness, or in rare cases, fainting. While often asymptomatic, the condition can become clinically significant during physical exertion when oxygen demand increases.
Diagnosis is usually made through coronary angiography, computed tomography, or intravascular imaging. These methods reveal the tunneled artery and determine the degree of compression on the affected vessel segment.
Treatment depends on symptom severity, ranging from lifestyle adjustments and medication to surgical intervention. Beta-blockers or calcium channel blockers reduce heart rate and contractility, while refractory cases may require surgery or stent placement.
| Medical Name | Myocardial Bridging (Myocardial Bridge) |
| Type | Congenital heart anomaly |
| Affected System | Cardiovascular system |
| Prevalence | Between 1 and 15% in the community; incidentally detected in most cases |
| Causes | Embedding of the coronary artery into the myocardium as a result of developmental anomalies |
| Symptoms | Chest pain, exertional angina, palpitations, fainting, rarely myocardial infarction |
| Diagnostic Methods | Coronary angiography, CT angiography, Stress ECHO, Invasive hemodynamic measurements |
| Treatment Methods | Medical treatment (beta blocker, calcium channel blocker), rarely surgery (myotomy) or stenting |
| Complications | Ischemic heart disease, arrhythmia, rarely sudden cardiac death |
| Observation | Medical treatment follow-up, periodic stress testing and monitoring |
What is Heart Muscle Band Disease (Myocardial Collapse)?
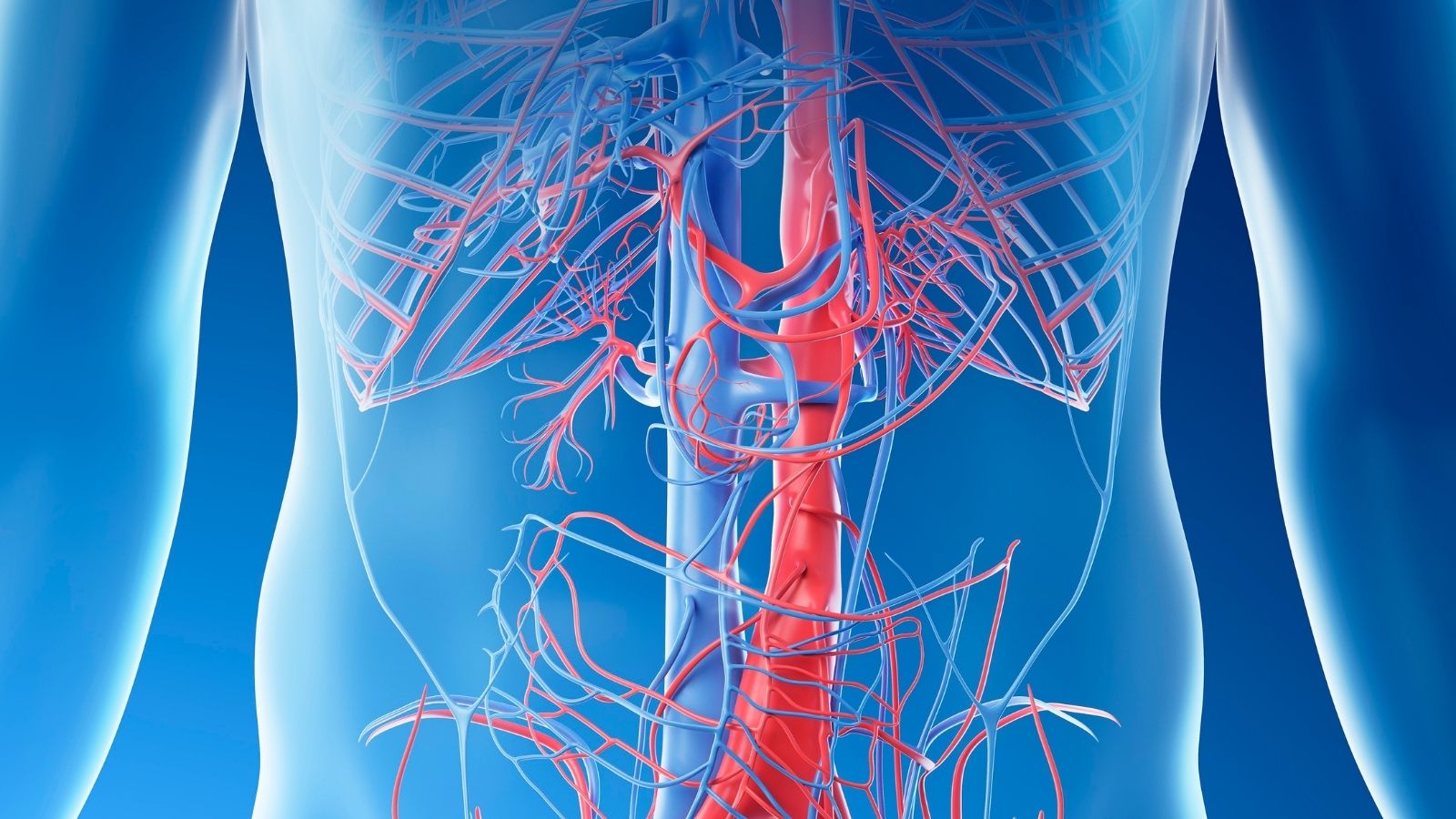
Our heart is a powerful muscle that never stops working, and it has its own network of blood vessels that supply it with oxygen and nutrients. We call these vessels coronary arteries. Normally, these arteries run along the outside of the heart muscle, like the branches of a tree spread out along the surface of its trunk. In some people, however, during development in the womb, one of these vessels, usually the left anterior descending artery (LAD), the most important vessel on the front of the heart, at some point plunges into the muscle, runs under the muscle for a short distance, and then comes back to the surface. We call this section where the vessel passes through the muscle tissue the “tunnel” and the muscle fibers that cover the vessel like a bridge the “myocardial bridge” or “muscle band”.
This should not be seen as the onset of a disease. It is an anatomical variation, just as some people have different eye color. Most of the time it’s completely harmless and doesn’t cause any problems in a person’s life. The problem starts when and only when this muscular bridge, especially when the heart is beating rapidly, significantly compresses the vessel passing underneath it, blocking the flow of blood. So there is no need for anyone hearing this diagnosis to immediately panic. It is important to carefully investigate whether this structural difference is the source of possible symptoms in the individual.
How common is Heart Muscle Band Disease in the community?
The frequency with which this occurs varies surprisingly depending on which method we use to detect it, and this difference actually tells us a lot about the nature of the situation.
In autopsy studies on deceased people, where the heart can be examined directly, cardiac muscle banding is very common. In some series, this rate can reach up to ‘s. This shows us how anatomically common this “bridge” structure actually is in society, almost a variant of the norm rather than an exception to the rule.
But when it comes to making a diagnosis in a living person, it is different. With the traditional method of coronary angiography, i.e. X-raying the vessels, the rate drops dramatically, with an incidence usually reported to be between 1% and 1%. Because angiography can only show cases where the vessel is significantly compressed when the heart contracts (the so-called “milking effect”). Today, thanks to more precise methods such as Coronary CT Angiography (CCTA), which provides detailed three-dimensional images of the heart and blood vessels, we can see these structures much more clearly. In CCTA scans, the incidence of myocardial deterioration is frequently above .
So what does the huge difference between these figures mean? This is not a contradiction but evidence of a very basic fact: Anatomically, having a muscle bridge is not the same as having a functional problem, that is, a problem that is significant enough to impair blood flow. Many people may have a small, superficial muscle band in the heart that is too small to cause symptoms or affect blood flow. Therefore, the diagnostic process does not end with just “finding the bridge”. What is important is to prove whether this restriction is “hemodynamically significant”, that is, whether it actually restricts blood flow to any significant extent.
How does Heart Muscle Band Disease affect the heart and blood vessels?
The effect of a cardiac muscle band on the body is more complex than simple mechanical compression. This can cause problems by affecting both the contraction and relaxation cycles of the heart and causing changes in the vessel wall over time.
The most well-known effect is that during contraction (systole), when the heart is pumping blood, the muscle band squeezes the underlying vessel like a vice. On angiography, this is seen as a “milking effect”, with a section of the vessel disappearing and reappearing. However, this is not the critical point. This is because the heart muscle meets most of its blood demand when it relaxes (diastole), not when it contracts.
The main problem with important muscle bridges is that this constricted vessel does not open quickly and quickly enough when the relaxation phase begins. this phenomenon, which we call “delayed diastolic relaxation”, means that it takes time for the vessel to reach its full capacity. This leads to insufficient blood flow when the heart’s blood supply is most important. This is the basic mechanism behind symptoms such as chest pain, which occurs when heart rate increases and the relaxation period is shortened, especially during exercise.
There is also an interesting dimension related to arteriosclerosis (atherosclerosis). Usually, the vascular segment just inside the muscle tunnel is protected from atherosclerosis because it is constantly exposed to external pressure, and plaque formation in this area is hardly visible. But as a paradox, the section just inside the bridge, i.e. before the blood enters the tunnel, is highly prone to developing atherosclerosis. This is because the blood experiences a turbulence in that area before entering the vein, the flow slows down and the forces exerted on the vessel wall change. These abnormal flow conditions damage the delicate layer lining the inside of the vessel (the endothelium), triggering plaque formation.
So why does a person live with this condition for years without any problems and then suddenly develop symptoms in middle age? This is usually not because the bridge has changed, but because the body has changed. Factors that have developed over the years, such as high blood pressure, thickening of the heart muscle, or a decrease in the heart’s overall ability to relax, can “surface” the effects of a previously tolerable muscle band. These additional factors increase the restriction of blood flow by the previously silent root, creating an imbalance in which the heart’s increased oxygen demand cannot be met and symptoms begin.
What symptoms can Heart Muscle Band Disease cause?
A large proportion of people with myocardial impairment are completely asymptomatic and live unaware of the condition. However, when the muscle band begins to affect the blood supply, some typical symptoms may occur, usually related to the heart muscle not getting enough oxygen (ischemia). The most common symptoms are the following:
- Sore chest (angina)
- Shortness of breath
- Distortion
- Excessive fatigue
- Head rotation
- Fainting sensation
This pain is usually described as a feeling of pressure, tightness or heaviness in the chest and is often triggered by exertion (climbing stairs, walking uphill, playing sports) or emotional stress. It is typical for it to be relieved at rest.
Does Cardiac Muscle Band Disease cause serious complications?
Although most muscle tears are benign, in rare cases, especially those that are anatomically very deep and long, they can cause serious problems. These risks are rare, but explain why symptomatic patients should be taken seriously. Potentially serious complications include the following:
- Heart attack (Myocardial Infarction)
- Life-threatening arrhythmias
- Stress cardiomyopathy (broken heart syndrome)
- Sudden cardiac death
The existence of these risks shows that symptoms should never be ignored and that proper diagnosis and treatment are crucial to prevent such undesirable outcomes.
How is the diagnosis of Heart Muscle Band Disease confirmed?
Diagnosing cardiac muscle bundle disease is like putting together the pieces of a jigsaw puzzle. The process aims not only to identify the anatomical defect, but more importantly, to prove whether this defect is really responsible for the patient’s symptoms. There are main diagnostic methods we use for this.
These methods usually start with non-invasive tests and continue with invasive tests if necessary. The main diagnostic tools are:
- Coronary CT Angiography (CCTA)
- Coronary Angiography
- Intravascular Ultrasound (IVUS)
- Diastolic Fractional Flow Reserve (dFFR)
Coronary CT Angiography (CCTA) is currently the most valuable and primary method of diagnosing this condition. By simply administering contrast material to the patient through a vein in the arm, this rapid CT scan produces a three-dimensional, incredibly detailed map of the heart and blood vessels. Thanks to CCTA, we can clearly see where the muscle band is, how long it is and the most critical information – its depth within the muscle. This is vital information both to confirm the diagnosis and to plan a possible surgery.
Coronary angiography is a classic method of accessing the heart via an artery in the groin or wrist. It supports the diagnosis by showing the compression of the vessel when the heart contracts, the so-called “milking effect”. However, on its own, it fails to show anatomical details, especially the thickness of the muscle and how deep the vessel is.
Intravascular Ultrasound (IVUS) is a very special procedure performed during angiography. It involves inserting a wire with a tiny ultrasound device at the end into the vessel, allowing us to see the vessel wall and surrounding muscle tissue from the inside. It clearly identifies the muscle tissue that appears like a “half-moon” over the vessel and provides invaluable anatomical information about the degree of compression.
Diastolic Fractional Flow Reserve (dFFR) is the most important test that reveals the functional dimension of the issue, i.e. gives a numerical answer to the question “Is this bridge really impairing blood flow?”. Also during angiography, a special pressure-sensitive wire is inserted into the vessel. The patient is then given a drug that speeds up the heartbeat and contraction, a kind of “effort test”. The difference in pressure between before and after the wire and the bridge is measured. If this difference falls below a set threshold (dFFRâ¤0.76), this proves that the bridge is clinically significant and that the patient’s symptoms are most likely caused by this bridge. This test is the most critical step in making a treatment decision.
Should everyone with Heart Muscle Band Disease be treated?
Absolutely not. A band of heart muscle that is detected incidentally during examinations for another reason and does not cause any discomfort to the person does not usually require special treatment. The vast majority of these people lead a normal life. The decision to treat is only made for patients who have symptoms and whose symptoms have been confirmed by tests to be due to a muscle worsening. However, lifestyle measures to maintain overall heart health and control of risk factors (blood pressure, cholesterol, smoking, etc.) are recommended for everyone diagnosed, even in the absence of symptoms.
What medication treatments are available for Heart Muscle Band Disease?
In symptomatic patients, the first line of treatment is usually medication. The aim is to reduce the compressive effect of the muscle band on the vessel by relieving the workload of the heart. The main groups of drugs used for this purpose are:
- Beta-blockers
- Calcium channel blockers (Non-dihydropyridine group)
These drugs slow the heart rate and slightly reduce the force with which the heart contracts. When the heart slows down, there is more time left for the relaxation (diastole) phase, which gives the squeezed vessel a longer time to fill with blood. The reduced contractile force also relieves the mechanical pressure on the vessel.
A very important warning must be made here: Patients with myocardial infarction should avoid nitrate-containing drugs (such as sublingual pills or sprays), known as vasodilators. These drugs, which are life-saving in normal vascular congestion, can worsen symptoms in this condition. This is because nitrates relax the vessel, making it easier to squeeze, and at the same time speed up the heart, increasing the squeezing effect. This can be a very dangerous combination.
Why is stenting (PCI) not usually preferred for the treatment of Heart Muscle Band Disease?
A stent, which is used to open a blocked vessel, is often not a good option for treating myocardial infarction. The problem is that the metal cage called a stent is subjected to a strong and dynamic muscle squeeze from the outside with every heartbeat. This is like putting a static structure up against a constantly moving force and leads to serious problems in the long run. These problems include:
- Stent fracture
- Re-narrowing in the stent (restenosis)
- Vascular puncture or rupture
The mechanical stress of constant compression can fatigue the metal structure of the stent over time, causing it to fracture. In addition, this constant trauma triggers an aggressive buildup of scar healing tissue within the stent, leading to very high rates and rapid recanalization of the vessel. For these reasons, stenting can only be considered as a last resort in very special and selected cases where there is no surgical option and no response to drug therapy.
When is surgical treatment for Heart Muscle Band Disease decided?
Surgical treatment is the surest solution, reserved for cases where drug therapy has failed. Surgery is usually decided for patients who meet the following criteria
- Symptoms that persist despite medication and seriously impair quality of life (e.g. chest pain even with small exertions).
- Severe impairment of blood supply (ischemia), which tests (especially dFFR) have proven to be due to a muscle wrist.
- Rarely, having had a heart attack or severe arrhythmia thought to be due to a muscle bridge.
How does myotomy (“Unroofing”) surgery eliminate Heart Muscle Band Disease?
Myotomy, also known colloquially as “roof lift”, is a surgical procedure that directly removes the root of the problem. The aim of this surgery is to surgically cut and separate the muscle band that is trapping the vein, leaving the vein completely free. Once the tunnel’s outlet is removed, the vessel is no longer squeezed every time the heart beats and the blood flow returns to normal. This is a very successful and safe procedure in experienced hands. Today, this surgery can be performed with different approaches.
- Median sternotomy (traditional open method)
- Minimally invasive surgery (small incisions)
- Robotic surgery
Minimally invasive methods, especially robotic surgery, offer smaller incisions, less pain and a faster recovery process, significantly improving patient comfort. Myotomy is the only treatment method that masks the problem or eliminates it permanently rather than temporarily resolving it.
When is Coronary Bypass (CABG) surgery an option in the treatment of Heart Muscle Band Disease?
Coronary bypass surgery is another surgical option that comes into play in certain situations where myotomy is not appropriate or safe. Bypass is based on the principle of creating an “alternative route” that goes around the problem rather than solving it. There are special cases where this surgery is preferred:
- The muscle bridge is too deep or too long.
- The attempted myotomy carries a risk of perforating the heart chamber.
- The presence of a severe and stable plaque of atherosclerosis immediately preceding the muscular rupture.
In these cases, instead of trying to release the muscle band, it may be safer and more effective to bypass the area and connect a new vessel (graft) that carries blood further up the vessel.
What should be the long-term expectation of someone with Heart Muscle Band Disease?
For the overwhelming majority of people with myocardial infarction, the long-term outlook (prognosis) is excellent. Most people have a completely normal life span and quality of life. The prognosis is particularly influenced by the presence of concomitant coronary artery disease and whether symptomatic patients receive the right treatment. Long-term outcomes, especially for symptomatic patients who have had a successful myotomy, are extremely gratifying in terms of relief from symptoms and improved quality of life.
What should be considered in lifestyle after a diagnosis of Cardiac Muscle Band Disease?
Once you have this diagnosis, it is very important to take steps to protect overall heart health, knowing that the risk of atherosclerosis is increased, especially in the pre-bridge area. Some positive changes in your life are the best investment in your long-term health. The most important points to be aware of are the following:
- Quit smoking immediately and completely
- Eating a heart-friendly diet (such as the Mediterranean diet)
- Regular physical activity (under doctor’s supervision)
- Maintaining ideal weight
- Keeping blood pressure under control
- Managing cholesterol levels
- Regular use of prescribed medicines
- Not neglecting doctor checks
- Monitor and report changes in symptoms
Frequently Asked Questions
What is myocardial bridge?
It is a congenital condition that occurs when the heart muscle is located in the shape of a bridge over a coronary artery.
How does this disease occur?
A section of the coronary artery, which normally runs on the surface, is embedded in the heart muscle. When the heart muscle contracts, this section of vessel is temporarily compressed.
Which coronary artery is most commonly affected?
The left anterior descending artery (LAD) is most commonly affected.
Is myocardial bridge dangerous?
Most of the time it is harmless, but in some people it can cause chest pain, arrhythmia and rarely sudden cardiac arrest.
What are the symptoms?
Chest pain, palpitations, dizziness and fainting may occur, which increase with exercise.
Does this disease cause heart attacks?
Rarely, it can cause a heart attack with coronary spasm or arrhythmia.
How is it diagnosed?
It is diagnosed by exercise testing, coronary CT angiography, conventional coronary angiography and intravascular ultrasound (IVUS).
Does every myocardial bridge require treatment?
No, patients without symptoms are usually only followed up.
What are the treatment options?
Medications such as beta-blockers and calcium channel blockers are used. Rarely, surgical treatment or a stent may be required.
When is surgical intervention performed?
In patients who do not respond to drug treatment and whose symptoms are severe, surgery called ‘myotomy’ can be performed.
Is this disease hereditary?
It is not thought to be hereditary; it is an innate structural condition.
Does it affect quality of life?
If severe symptoms are present, it can reduce quality of life; however, most people can lead normal lives.
Is exercise harmful?
Light exercise is generally safe; activities that cause symptoms should be avoided.
Can myocardial bridge be associated with other heart diseases?
Yes, it can be associated with coronary artery disease and rhythm disturbances.

Prof. Dr. Yavuz Beşoğul graduated from Erciyes University Faculty of Medicine in 1989 and completed his specialization in Cardiovascular Surgery in 1996. Between 1997 and 2012, he served at Eskişehir Osmangazi University Faculty of Medicine as Assistant Professor, Associate Professor, and Professor, respectively. Prof. Dr. Beşoğul, one of the pioneers of minimally invasive cardiovascular surgery in Türkiye, has specialized in closed-heart surgeries, underarm heart valve surgery, beating-heart bypass, and peripheral vascular surgery. He worked at Florence Nightingale Kızıltoprak Hospital between 2012–2014, Medicana Çamlıca Hospital between 2014–2017, and İstinye University (Medical Park) Hospital between 2017–2023. With over 100 publications and one book chapter, Prof. Dr. Beşoğul has contributed significantly to the medical literature and is known for his minimally invasive approaches that prioritize patient safety and rapid recovery.